|
英文药名:Xylocaine MPF(lidocaine HCl Injection, USP)
中文药名:盐酸利多卡因注射液
生产厂家:APP制药
药品介绍
本品是应用广泛的中效酰胺类局麻药,因其脂溶性、蛋白结合率都比普鲁卡因高,穿透细胞的能力强,所以它比普鲁卡因起效快、作用时间长,作用强度是普鲁卡因的4倍。利多卡因对各种病因引起的心动过速有效率高达80%以上,且较安全。因此利多卡因可作为各种病因引起的急性室性心律失常的首选药物。
XYLOCAINE MPF(lidocaine hydrochloride)injection, solution
For Infiltration and Nerve Block.
Rx only
DESCRIPTION
Xylocaine (lidocaine HCl) Injections are sterile, nonpyrogenic,aqueous solutions that contain a local anesthetic agent with or withoutepinephrine and are administered parenterally by injection. See INDICATIONS for specificuses.
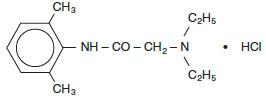
Xylocaine solutions contain lidocaine HCl, which is chemicallydesignated as acetamide, 2-(diethylamino)-N-(2,6-dimethylphenyl)-,monohydrochloride and has the molecular wt. 270.8. Lidocaine HCl(C14H22N2O • HCl) has thefollowing structural formula:
Epinephrine is (-) -3, 4-Dihydroxy-α-[(methylamino) methyl]benzyl alcohol and has the molecular wt. 183.21. Epinephrine(C9H13NO3) has the followingstructural formula:

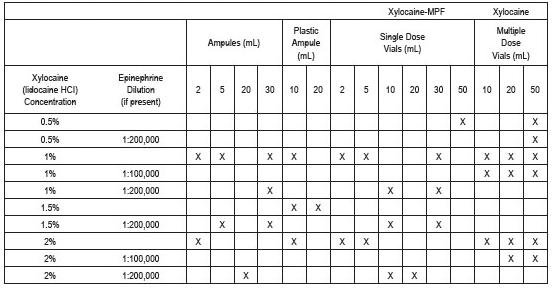
Dosage forms listed as Xylocaine-MPF indicate single dose solutions that are Methyl Paraben Free (MPF).
Xylocaine-MPF is a sterile, nonpyrogenic,isotonic solution containing sodium chloride. Xylocaine in multiple dose vials, each mL also contains 1 mg methylparaben as antisepticpreservative. The pH of these solutions is adjusted toapproximately 6.5 (5.0 to 7.0) with sodium hydroxide and/or hydrochloricacid.
Xylocaine-MPF with Epinephrine is asterile, nonpyrogenic, isotonic solution containing sodiumchloride. Each mL contains lidocaine hydrochloride andepinephrine, with 0.5 mg sodium metabisulfite as an antioxidant and 0.2mg citric acid as a stabilizer. Xylocaine withEpinephrine in multiple dose vials, each mL also contains 1 mg methylparaben as antisepticpreservative. The pH of these solutions is adjusted toapproximately 4.5 (3.3 to 5.5) with sodium hydroxide and/or hydrochloricacid. Filled under nitrogen.
CLINICAL PHARMACOLOGY
Mechanism of Action
Lidocaine stabilizes the neuronal membrane byinhibiting the ionic fluxes required for the initiation andconduction of impulses thereby effecting local anestheticaction.
Hemodynamics
Excessive blood levels may cause changes in cardiac output, total peripheral resistance, and mean arterial pressure. With central neural blockade these changes may be attributable to block of autonomic fibers, a direct depressant effect of the local anesthetic agent on various components of the cardiovascular system, and/or the beta-adrenergic receptor stimulating action of epinephrine when present. The net effect is normally a modest hypotension when the recommended dosages are not exceeded.
Pharmacokinetics and Metabolism
Information derived from diverse formulations,concentrations and usages reveals that lidocaine iscompletely absorbed following parenteral administration, itsrate of absorption depending, for example, upon various factorssuch as the site of administration and the presence or absenceof a vasoconstrictor agent. Except for intravascularadministration, the highest blood levels are obtained followingintercostal nerve block and the lowest after subcutaneousadministration.
The plasma binding of lidocaine is dependent on drugconcentration, and the fraction bound decreases with increasingconcentration. At concentrations of 1 to 4 mcg of freebase per mL 60 to 80 percent of lidocaine is proteinbound. Binding is also dependent on the plasmaconcentration of the alpha-1-acid glycoprotein.
Lidocaine crosses the blood-brain and placentalbarriers, presumably by passive diffusion.
Lidocaine is metabolized rapidly by the liver, andmetabolites and unchanged drug are excreted by thekidneys. Biotransformation includes oxidativeN-dealkylation, ring hydroxylation, cleavage of the amidelinkage, and conjugation. N-dealkylation, a major pathwayof biotransformation, yields the metabolitesmonoethylglycinexylidide and glycinexylidide. Thepharmacological/toxicological actions of these metabolites aresimilar to, but less potent than, those of lidocaine.Approximately 90% of lidocaine administered is excretedin the form of various metabolites, and less than 10% isexcreted unchanged. The primary metabolite in urine is aconjugate of 4-hydroxy-2,6-dimethylaniline.
The elimination half-life of lidocaine following anintravenous bolus injection is typically 1.5 to 2 hours.Because of the rapid rate at which lidocaine is metabolized,any condition that affects liver function may alter lidocaine kinetics. The half-life may be prolonged two-fold ormore in patients with liver dysfunction. Renal dysfunctiondoes not affect lidocaine kinetics but may increase theaccumulation of metabolites.
Factors such as acidosis and the use of CNS stimulantsand depressants affect the CNS levels of lidocaine requiredto produce overt systemic effects. Objective adversemanifestations become increasingly apparent with increasingvenous plasma levels above 6 mcg free base per mL. In therhesus monkey arterial blood levels of 18 to 21 mcg/mL have beenshown to be threshold for convulsive activity.
INDICATIONS AND USAGE
Xylocaine (lidocaine HCl) Injections are indicated for production of local or regional anesthesia by infiltration techniques such as percutaneous injection and intravenous regional anesthesia by peripheral nerve block techniques such as brachial plexus and intercostal and by central neural techniques such as lumbar and caudal epidural blocks, when the accepted procedures for these techniques as described in standard textbooks are observed.
CONTRAINDICATIONS
Lidocaine is contraindicated in patients with a known historyof hypersensitivity to local anesthetics of the amide type.
WARNINGS
XYLOCAINE INJECTIONS FOR INFILTRATION AND NERVE BLOCK SHOULD BEEMPLOYED ONLY BY CLINICIANS WHO ARE WELL VERSED IN DIAGNOSIS ANDMANAGEMENT OF DOSE-RELATED TOXICITY AND OTHER ACUTE EMERGENCIES THATMIGHT ARISE FROM THE BLOCK TO BE EMPLOYED AND THEN ONLY AFTER ENSURINGTHE IMMEDIATE AVAILABILITY OF OXYGEN, OTHERRESUSCITATIVE DRUGS, CARDIOPULMONARY EQUIPMENT AND THE PERSONNEL NEEDEDFOR PROPER MANAGEMENT OF TOXIC REACTIONS AND RELATED EMERGENCIES. (Seealso ADVERSEREACTIONS and PRECAUTIONS.) DELAY INPROPER MANAGEMENT OF DOSE-RELATED TOXICITY, UNDERVENTILATION FROM ANYCAUSE AND/OR ALTERED SENSITIVITY MAY LEAD TO THE DEVELOPMENT OFACIDOSIS, CARDIAC ARREST AND, POSSIBLY, DEATH.
Intra-articular infusions of local anesthetics followingarthroscopic and other surgical procedures is an unapproved use, andthere have been post-marketing reports of chondrolysis in patientsreceiving such infusions. The majority of reported cases ofchondrolysis have involved the shoulder joint; cases of gleno-humeralchondrolysis have been described in pediatric and adult patientsfollowing intra-articular infusions of local anesthetics with andwithout epinephrine for periods of 48 to 72 hours. There isinsufficient information to determine whether shorter infusion periodsare not associated with these findings. The time of onset ofsymptoms, such as joint pain, stiffness and loss of motion can bevariable, but may begin as early as the 2nd month after surgery.Currently, there is no effective treatment for chondrolysis; patientswho experienced chondrolysis have required additional diagnostic andtherapeutic procedures and some required arthroplasty or shoulderreplacement.
To avoid intravascular injection, aspiration should be performedbefore the local anesthetic solution is injected. The needle mustbe repositioned until no return of blood can be elicited byaspiration. Note, however, that the absence of blood in thesyringe does not guarantee that intravascular injection has beenavoided.
Local anesthetic solutions containing antimicrobial preservatives(e.g., methylparaben) should not be used for epidural or spinal anesthesiabecause the safety of these agents has not been established with regardto intrathecal injection, either intentional or accidental.
Xylocaine with epinephrine solutions contain sodiummetabisulfite, a sulfite that may cause allergic-type reactionsincluding anaphylactic symptoms and life-threatening or less severeasthmatic episodes in certain susceptible people. The overallpreva lence of sulfite sensitivity in the general population is unknownand probably low. Sulfite sensitivity is seen more frequently inasthmatic than in non-asthmatic people.
PRECAUTIONS
General
The safety and effectiveness of lidocaine depend onproper dosage, correct technique, adequate precautions, andreadiness for emergencies. Standard textbooks should beconsulted for specific techniques and precautions for variousregional anesthetic procedures.
Resuscitative equipment, oxygen, and other resuscitativedrugs should be available for immediate use (see WARNINGS and ADVERSEREACTIONS). Thelowest dosage that results in effective anesthesia should beused to avoid high plasma levels and serious adverseeffects. Syringe aspirations should also be performedbefore and during each supplemental injection when usingindwelling catheter techniques. During the administrationof epidural anesthesia, it is recommended that a test dose beadministered initially and that the patient be monitored forcentral nervous system toxicity and cardiovascular toxicity, aswell as for signs of unintended intrathecal administration,before proceeding. When clinical conditions permit,consideration should be given to employing local anestheticsolutions that contain epinephrine for the test dose becausecirculatory changes compatible with epinephrine may also serveas a warning sign of unintended intravascular injection.An intravascular injection is still possible even if aspirationsfor blood are negative. Repeated doses of lidocainemay cause significant increases in blood levels with eachrepeated dose because of slow accumulation of the drug or itsmetabolites. Tolerance to elevated blood levels varieswith the status of the patient. Debilitated, elderlypatients, acutely ill patients, and children should be givenreduced doses commensurate with their age and physicalcondition. Lidocaine should also be used with cautionin patients with severe shock or heart block.
Lumbar and caudal epidural anesthesia should be used withextreme caution in persons with the following conditions:existing neurological disease, spinal deformities, septicemia,and severe hypertension.
Local anesthetic solutions containing a vasoconstrictorshould be used cautiously and in carefully circumscribedquantities in areas of the body supplied by end arteries orhaving otherwise compromised blood supply. Patients withperipheral vascular disease and those with hypertensive vasculardisease may exhibit exaggerated vasoconstrictor response.Ischemic injury or necrosis may result. Preparationscontaining a vasoconstrictor should be used with caution inpatients during or following the administration of potentgeneral anesthetic agents, since cardiac arrhythmias may occurunder such conditions.
Careful and constant monitoring of cardiovascular andrespiratory (adequacy of ventilation) vital signs and thepatient’s state of consciousness should be accomplishedafter each local anesthetic injection. It should be keptin mind at such times that restlessness, anxiety, tinnitus,dizziness, blurred vision, tremors, depression or drowsiness maybe early warning signs of central nervous systemtoxicity.
Since amide-type local anesthetics are metabolized by theliver, Xylocaine Injection should be used with caution inpatients with hepatic disease. Patients with severehepatic disease, because of their inability to metabolize localanesthetics normally, are at greater risk of developing toxicplasma concentrations. Xylocaine Injection should also beused with caution in patients with impaired cardiovascularfunction since they may be less able to compensate forfunctional changes associated with the prolongation of A-Vconduction produced by these drugs.
Many drugs used during the conduct of anesthesia areconsidered potential triggering agents for familial malignanthyperthermia. Since it is not known whether amide-typelocal anesthetics may trigger this reaction and since the needfor supplemental general anesthesia cannot be predicted inadvance, it is suggested that a standard protocol for themanagement of malignant hyperthermia should be available.Early unexplained signs of tachycardia, tachypnea, labile bloodpressure and metabolic acidosis may precede temperatureelevation. Successful outcome is dependent on earlydiagnosis, prompt discontinuance of the suspect triggeringagent(s) and institution of treatment, including oxygen therapy,indicated supportive measures and dantrolene (consult dantrolenesodium intravenous package insert before using).
Proper tourniquet technique, as described in publicationsand standard textbooks, is essential in the performance ofintravenous regional anesthesia. Solutions containingepinephrine or other vasoconstrictors should not be used forthis technique.
Lidocaine should be used with caution in persons withknown drug sensitivities. Patients allergic topara-aminobenzoic acid derivatives (procaine, tetracaine,benzocaine, etc.) have not shown cross sensitivity to lidocaine.
Use in the Head and Neck Area
Small doses of local anesthetics injected into the head and neck area, including retrobulbar, dental and stellate ganglion blocks, may produce adverse reactions similar to systemic toxicity seen with unintentional intravascular injections of larger doses. Confusion, convulsions, respiratory depression and/or respiratory arrest, and cardiovascular stimulation or depression have been reported. These reactions may be due to intra-arterial injection of the local anesthetic with retrograde flow to the cerebral circulation. Patients receiving these blocks should have their circulation and respiration monitored and be constantly observed. Resuscitative equipment and personnel for treating adverse reactions should be immediately available. Dosage recommendations should not be exceeded (see DOSAGE AND ADMINISTRATION).
Information for Patients
When appropriate, patients should be informed in advance that they may experience temporary loss of sensation and motor activity, usually in the lower half of the body, following proper administration of epidural anesthesia.
Clinically Significant Drug Interactions
The administration of local anesthetic solutions containing epinephrine or norepinephrine to patients receiving monoamine oxidase inhibitors or tricyclic antidepressants may produce severe, prolonged hypertension.
Phenothiazines and butyrophenones may reduce or reverse the pressor effect of epinephrine.
Concurrent use of these agents should generally be avoided. In situations when concurrent therapy is necessary, careful patient monitoring is essential.
Concurrent administration of vasopressor drugs (for the treatment of hypotension related to obstetric blocks) and ergot-type oxytocic drugs may cause severe, persistent hypertension or cerebrovascular accidents.
Drug/Laboratory Test Interactions
The intramuscular injection of lidocaine may resultin an increase in creatine phosphokinase levels. Thus, theuse of this enzyme determination, without isoenzyme separation,as a diagnostic test for the presence of acute myocardialinfarction may be compromised by the intramuscular injection oflidocaine.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies of lidocaine in animals to eva luate thecarcinogenic and mutagenic potential or the effect on fertilityhave not been conducted.
Pregnancy
Teratogenic Effects: Pregnancy Category B.Reproduction studies have been performed in rats at doses up to6.6 times the human dose and have revealed no evidence of harmto the fetus caused by lidocaine. There are, however,no adequate and well-controlled studies in pregnant women.Animal reproduction studies are not always predictive of humanresponse. General consideration should be given to thisfact before administering lidocaine to women of childbearingpotential, especially during early pregnancy when maximumorganogenesis takes place.
Labor and Delivery
Local anesthetics rapidly cross the placenta and whenused for epidural, paracervical, pudendal or caudal blockanesthesia, can cause varying degrees of maternal, fetal andneonatal toxicity (see CLINICAL PHARMACOLOGY, Pharmacokinetics).The potential for toxicity depends upon the procedure performed,the type and amount of drug used, and the technique of drugadministration. Adverse reactions in the parturient, fetusand neonate involve alterations of the central nervous system,peripheral vascular tone and cardiac function.
Maternal hypotension has resulted from regionalanesthesia. Local anesthetics produce vasodilation byblocking sympathetic nerves. Elevating the patient’slegs and positioning her on her left side will help preventdecreases in blood pressure.
The fetal heart rate also should be monitoredcontinuously, and electronic fetal monitoring is highlyadvisable.
Epidural, spinal, paracervical, or pudendal anesthesiamay alter the forces of parturition through changes in uterinecontractility or maternal expulsive efforts. In one study,paracervical block anesthesia was associated with a decrease inthe mean duration of first stage labor and facilitation ofcervical dilation. However, spinal and epidural anesthesiahave also been reported to prolong the second stage of labor byremoving the parturient’s reflex urge to bear down or byinterfering with motor function. The use of obstetricalanesthesia may increase the need for forcepsassistance.
The use of some local anesthetic drug products duringlabor and delivery may be followed by diminished muscle strengthand tone for the first day or two of life. The long-termsignificance of these observations is unknown. Fetalbradycardia may occur in 20 to 30 percent of patients receivingparacervical nerve block anesthesia with the amide-type localanesthetics and may be associated with fetal acidosis.Fetal heart rate should always be monitored during paracervicalanesthesia. The physician should weigh the possibleadvantages against risks when considering a paracervical blockin prematurity, toxemia of pregnancy, and fetal distress.Careful adherence to recommended dosage is of the utmostimportance in obstetrical paracervical block. Failure toachieve adequate analgesia with recommended doses should arousesuspicion of intravascular or fetal intracranialinjection. Cases compatible with unintended fetalintracranial injection of local anesthetic solution have beenreported following intended paracervical or pudendal block orboth. Babies so affected present with unexplained neonataldepression at birth, which correlates with high local anestheticserum levels, and often manifest seizures within sixhours. Prompt use of supportive measures combined withforced urinary excretion of the local anesthetic has been usedsuccessfully to manage this complication.
Case reports of maternal convulsions and cardiovascularcollapse following use of some local anesthetics forparacervical block in early pregnancy (as anesthesia forelective abortion) suggest that systemic absorption under thesecircumstances may be rapid. The recommended maximum doseof each drug should not be exceeded. Injection should bemade slowly and with frequent aspiration. Allow a 5-minuteinterval between sides.
Nursing Mothers
It is not known whether this drug is excreted in humanmilk. Because many drugs are excreted in human milk,caution should be exercised when lidocaine is administeredto a nursing woman.
Pediatric Use
Dosages in children should be reduced, commensurate withage, body weight and physical condition (see DOSAGEANDADMINISTRATION).
ADVERSE REACTIONS
Systemic
Adverse experiences following the administration oflidocaine are similar in nature to those observed with otheramide local anesthetic agents. These adverse experiencesare, in general, dose-related and may result from high plasmalevels caused by excessive dosage, rapid absorption orinadvertent intravascular injection, or may result from ahypersensitivity, idiosyncrasy or diminished tolerance on thepart of the patient. Serious adverse experiences aregenerally systemic in nature. The following types arethose most commonly reported:
Central Nervous System
CNS manifestations are excitatory and/or depressant andmay be characterized by lightheadedness, nervousness,apprehension, euphoria, confusion, dizziness, drowsiness,tinnitus, blurred or double vision, vomiting, sensations ofheat, cold or numbness, twitching, tremors, convulsions,unconsciousness, respiratory depression and arrest. Theexcitatory manifestations may be very brief or may not occur atall, in which case the first manifestation of toxicity may bedrowsiness merging into unconsciousness and respiratoryarrest.
Drowsiness following the administration of lidocaineis usually an early sign of a high blood level of the drug andmay occur as a consequence of rapid absorption.
Cardiovascular System
Cardiovascular manifestations are usually depressant and are characterized by bradycardia, hypotension, and cardiovascular collapse, which may lead to cardiac arrest.
Allergic
Allergic reactions are characterized by cutaneouslesions, urticaria, edema or anaphylactoid reactions.Allergic reactions may occur as a result of sensitivity eitherto local anesthetic agents or to the methylparaben used as apreservative in the multiple dose vials. Allergicreactions as a result of sensitivity to lidocaine areextremely rare and, if they occur, should be managed byconventional means. The detection of sensitivity by skintesting is of doubtful value.
Neurologic
The incidences of adverse reactions associated with theuse of local anesthetics may be related to the total dose oflocal anesthetic administered and are also dependent upon theparticular drug used, the route of administration and thephysical status of the patient. In a prospective review of10,440 patients who received lidocaine for spinalanesthesia, the incidences of adverse reactions were reported tobe about 3 percent each for positional headaches, hypotensionand backache; 2 percent for shivering; and less than 1 percenteach for peripheral nerve symptoms, nausea, respiratoryinadequacy and double vision. Many of these observationsmay be related to local anesthetic techniques, with or without acontribution from the local anesthetic.
In the practice of caudal or lumbar epidural block,occasional unintentional penetration of the subarachnoid spaceby the catheter may occur. Subsequent adverse effects maydepend partially on the amount of drug administeredsubdurally. These may include spinal block of varyingmagnitude (including total spinal block), hypotension secondaryto spinal block, loss of bladder and bowel control, and loss ofperineal sensation and sexual function. Persistent motor,sensory and/or autonomic (sphincter control) deficit of somelower spinal segments with slow recovery (several months) orincomplete recovery have been reported in rare instances whencaudal or lumbar epidural block has been attempted.Backache and headache have also been noted following use ofthese anesthetic procedures.
There have been reported cases of permanent injury toextraocular muscles requiring surgical repair followingretrobulbar administration.
OVERDOSAGE
Acute emergencies from local anesthetics are generally related to high plasma levels encountered during therapeutic use of local anesthetics or to unintended subarachnoid injection of local anesthetic solution (see ADVERSE REACTIONS, WARNINGS, and PRECAUTIONS).
Management of Local Anesthetic Emergencies
The first consideration is prevention, best accomplishedby careful and constant monitoring of cardiovascular andrespiratory vital signs and the patient’s state ofconsciousness after each local anesthetic injection. Atthe first sign of change, oxygen should beadministered.
The first step in the management of convulsions, as wellas underventilation or apnea due to unintended subarachnoidinjection of drug solution, consists of immediate attention tothe maintenance of a patent airway and assisted or controlledventilation with oxygen and a delivery system capable ofpermitting immediate positive airway pressure by mask.Immediately after the institution of these ventilatory measures,the adequacy of the circulation should be eva luated, keeping inmind that drugs used to treat convulsions sometimes depress thecirculation when administered intravenously. Shouldconvulsions persist despite adequate respiratory support, and ifthe status of the circulation permits, small increments of anultra-short acting barbiturate (such as thiopental or thiamylal)or a benzodiazepine (such as diazepam) may be administeredintravenously. The clinician should be familiar, prior tothe use of local anesthetics, with these anticonvulsantdrugs. Supportive treatment of circulatory depression mayrequire administration of intravenous fluids and, whenappropriate, a vasopressor as directed by the clinical situation(e.g., ephedrine).
If not treated immediately, both convulsions andcardiovascular depression can result in hypoxia, acidosis,bradycardia, arrhythmias and cardiac arrest.Underventilation or apnea due to unintentional subarachnoidinjection of local anesthetic solution may produce these samesigns and also lead to cardiac arrest if ventilatory support isnot instituted. If cardiac arrest should occur, standardcardiopulmonary resuscitative measures should beinstituted.
Endotracheal intubation, employing drugs and techniquesfamiliar to the clinician, may be indicated, after initialadministration of oxygen by mask, if difficulty is encounteredin the maintenance of a patent airway or if prolongedventilatory support (assisted or controlled) isindicated.
Dialysis is of negligible value in the treatment of acuteoverdosage with lidocaine.
The oral LD50 of lidocaine in non-fastedfemale rats is 459 (346 to 773) mg/kg (as the salt) and 214 (159to 324) mg/kg (as the salt) in fasted female rats.
DOSAGE AND ADMINISTRATION
Table 1 (Recommended Dosages) summarizes the recommended volumesand concentrations of Xylocaine Injection for various types ofanesthetic procedures. The dosages suggested in this table are fornormal healthy adults and refer to the use of epinephrine-freesolutions. When larger volumes are required, only solutionscontaining epinephrine should be used except in those cases wherevasopressor drugs may be contraindicated.
There have been adverse event reports of chondrolysis in patientsreceiving intra-articular infusions of local anesthetics followingarthroscopic and other surgical procedures. Xylocaine is notapproved for this use (see WARNINGS and DOSAGE ANDADMINISTRATION).
These recommended doses serve only as a guide to the amount ofanesthetic required for most routine procedures. The actualvolumes and concentrations to be used depend on a number of factors suchas type and extent of surgical procedure, depth of anesthesia and degreeof muscular relaxation required, duration of anesthesia required, andthe physical condition of the patient. In all cases the lowestconcentration and smallest dose that will produce the desired resultshould be given. Dosages should be reduced for children and forthe elderly and debilitated patients and patients with cardiac and/orliver disease.
The onset of anesthesia, the duration of anesthesia and thedegree of muscular relaxation are proportional to the volume andconcentration (i.e., total dose) of local anesthetic used. Thus, anincrease in volume and concentration of Xylocaine Injection willdecrease the onset of anesthesia, prolong the duration of anesthesia,provide a greater degree of muscular relaxation and increase thesegmental spread of anesthesia. However, increasing the volume andconcentration of Xylocaine Injection may result in a more profound fallin blood pressure when used in epidural anesthesia. Although theincidence of side effects with lidocaine is quite low, cautionshould be exercised when employing large volumes and concentrations,since the incidence of side effects is directly proportional to thetotal dose of local anesthetic agent injected.
For intravenous regional anesthesia, only the 50 mL single dosevial containing Xylocaine (lidocaine HCl) 0.5% Injection should beused.
Epidural Anesthesia
For epidural anesthesia, only the following dosage formsof Xylocaine Injection are recommended:
1% withoutepinephrine 10 mL Plastic Ampule
1% withoutepinephrine 30 mL single dose solutions
1% withepinephrine 1:200,000 30 mL single dose solutions
1.5% withoutepinephrine 10 mL Plastic Ampule
1.5% withoutepinephrine20 mL Plastic Ampule
1.5% withepinephrine 1:200,000 30 mL ampules, 30 mL single dose solutions
2% withoutepinephrine10 mL Plastic Ampule
2% withepinephrine 1:200,000 20 mL ampules, 20 mL single dose solutions
Although these solutions are intended specifically forepidural anesthesia, they may also be used for infiltration andperipheral nerve block, provided they are employed as singledose units. These solutions contain no bacteriostaticagent.
In epidural anesthesia, the dosage varies with thenumber of dermatomes to be anesthetized (generally 2 to 3 mL ofthe indicated concentration per dermatome).
Caudal and Lumbar Epidural Block
As a precaution against the adverse experience sometimesobserved following unintentional penetration of the subarachnoidspace, a test dose such as 2 to 3 mL of 1.5% lidocaineshould be administered at least 5 minutes prior to injecting thetotal volume required for a lumbar or caudal epiduralblock. The test dose should be repeated if the patient ismoved in a manner that may have displaced the catheter.Epinephrine, if contained in the test dose (10 to 15 mcg havebeen suggested), may serve as a warning of unintentionalintravascular injection. If injected into a blood vessel,this amount of epinephrine is likely to produce a transient“epinephrine response” within 45 seconds, consistingof an increase in heart rate and systolic blood pressure,circumoral pallor, palpitations and nervousness in the unsedatedpatient. The sedated patient may exhibit only a pulse rateincrease of 20 or more beats per minute for 15 or moreseconds. Patients on beta blockers may not manifestchanges in heart rate, but blood pressure monitoring can detectan evanescent rise in systolic blood pressure. Adequatetime should be allowed for onset of anesthesia afteradministration of each test dose. The rapid injection of alarge volume of Xylocaine Injection through the catheter shouldbe avoided, and, when feasible, fractional doses should beadministered.
In the event of the known injection of a large volume oflocal anesthetic solution into the subarachnoid space, aftersuitable resuscitation and if the catheter is in place, considerattempting the recovery of drug by draining a moderate amount ofcerebrospinal fluid (such as 10 mL) through the epiduralcatheter.
MAXIMUM RECOMMENDED DOSAGES
Adults
For normal healthy adults, the individual maximumrecommended dose of lidocaine HCl with epinephrine should notexceed 7 mg/kg (3.5 mg/lb) of body weight, and in general it isrecommended that the maximum total dose not exceed 500 mg.When used without epinephrine the maximum individual dose shouldnot exceed 4.5 mg/kg (2 mg/lb) of body weight, and in general itis recommended that the maximum total dose does not exceed 300mg. For continuous epidural or caudal anesthesia, themaximum recommended dosage should not be administered atintervals of less than 90 minutes. When continuous lumbaror caudal epidural anesthesia is used for non-obstetricalprocedures, more drug may be administered if required to produceadequate anesthesia.
The maximum recommended dose per 90 minute period oflidocaine hydrochloride for paracervical block in obstetricalpatients and non-obstetrical patients is 200 mg total. Onehalf of the total dose is usually administered to each side. Inject slowly, five minutes between sides. (See also discussionof paracervical block in PRECAUTIONS.)
For intravenous regional anesthesia, the doseadministered should not exceed 4 mg/kg in adults.
Children
It is difficult to recommend a maximum dose of any drugfor children, since this varies as a function of age andweight. For children over 3 years of age who have a normallean body mass and normal body development, the maximum dose isdetermined by the child’s age and weight. Forexample, in a child of 5 years weighing 50 lbs the dose oflidocaine HCl should not exceed 75 to 100 mg (1.5 to 2mg/lb). The use of even more dilute solutions (i.e., 0.25 to0.5%) and total dosages not to exceed 3 mg/kg (1.4 mg/lb)are recommended for induction of intravenous regional anesthesiain children.
In order to guard against systemic toxicity, the lowesteffective concentration and lowest effective dose should be usedat all times. In some cases it will be necessary to diluteavailable concentrations with 0.9% sodium chloride injectionin order to obtain the required final concentration.
NOTE: Parenteral drug products should be inspectedvisually for particulate matter and discoloration prior toadministration whenever the solution and container permit.The Injection is not to be used if its color is pinkish ordarker than slightly yellow or if it contains aprecipitate.
Table 1: Recommended Dosages
Procedure |
Xylocaine (lidocaine hydrochloride)
Injection (without epinephrine) |
|
Conc (%) |
Vol (mL) |
Total Dose (mg) |
|
Infiltration |
|
Percutaneous |
0.5 or 1 |
1 to 60 |
5 to 300 |
|
Intravenous regional |
0.5 |
10 to 60 |
50 to 300 |
|
Peripheral Nerve Blocks, e.g. |
|
Brachial |
1.5 |
15 to 20 |
225 to 300 |
|
Dental |
2 |
1 to 5 |
20 to 100 |
|
Intercostal |
1 |
3 |
30 |
|
Paravertebral |
1 |
3 to 5 |
30 to 50 |
|
Pudendal (each side) |
1 |
10 |
100 |
|
Paracervical |
|
Obstetrical analgesia (each side) |
1
|
10
|
100
|
|
Sympathetic Nerve Blocks, e.g. |
|
Cervical (stellate ganglion) |
1 |
5 |
50 |
|
Lumbar |
1 |
5 to 10 |
50 to 100 |
|
Central Neural Blocks |
|
Epidural* |
|
Thoracic |
1 |
20 to 30 |
200 to 300 |
|
Lumbar |
|
Analgesia |
1 |
25 to 30 |
250 to 300 |
|
Anesthesia |
1.5 |
15 to 20 |
225 to 300 |
|
2 |
10 to 15 |
200 to 300 |
|
Caudal |
|
Obstetrical analgesia |
1 |
20 to 30 |
200 to 300 |
|
Surgical anesthesia |
1.5 |
15 to 20 |
225 to 300 |
*Dose determined by number of dermatomes to beanesthetized (2 to 3 mL/dermatome).
THE ABOVE SUGGESTED CONCENTRATIONS AND VOLUMES SERVE ONLYAS A GUIDE. OTHER VOLUMES AND CONCENTRATIONS MAY BE USEDPROVIDED THE TOTAL MAXIMUM RECOMMENDED DOSE IS NOTEXCEEDED.
STERILIZATION, STORAGE AND TECHNICAL PROCEDURES
Disinfecting agents containing heavy metals, which cause releaseof respective ions (mercury, zinc, copper, etc.) should not be used forskin or mucous membrane disinfection as they have been related toincidents of swelling and edema. When chemical disinfection ofmulti-dose vials is desired, either isopropyl alcohol (91%) or ethylalcohol (70%) is recommended. Many commercially availablebrands of rubbing alcohol, as well as solutions of ethyl alcohol not ofU.S.P. grade, contain denaturants which are injurious to rubber andtherefore are not to be used.
Dosage forms listed as Xylocaine-MPF indicate single dosesolutions that are Methyl Paraben Free(MPF).
HOW SUPPLIED
All solutions should be stored at 20° to 25°C (68°to 77°F) [see USP Controlled Room Temperature].
PACKAGE LABEL – PRINCIPAL DISPLAY – Xylocaine - MPF 10 mL Ampule Label
NDC 63323-492-97
491297
Xylocaine® - MPF (lidocaine HCl Injection, USP)
1% (10 mg/mL)
Not For Inhalation.
10 mL ampule
Rx only

PACKAGE LABEL – PRINCIPALDISPLAY – Xylocaine - MPF 10 mL Ampule Lidding Label
NDC 63323-492-97
491297
Xylocaine® - MPF (lidocaine HCl Injection,USP)
1% (10 mg/mL)
For Infiltration and Nerve Block Including Caudal and Epidural Use.
Not For Inhalation.
Methylparaben Free
Rx only

PACKAGE LABEL – PRINCIPALDISPLAY – Xylocaine - MPF 10 mL Ampule CartonPanel
NDC 63323-492-97
491297
Xylocaine® - MPF (lidocaine HCl Injection,USP)
1% (10 mg/mL)
For Infiltration and Nerve Block Including Caudal and EpiduralUse.
Not For Inhalation.
Methylparaben Free
Rx only
Sterile-Pak
Contains Five Presterilized
10 mL Plastic Ampule Units

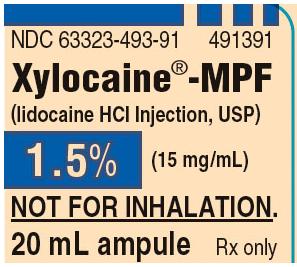
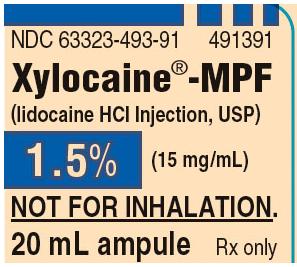
PACKAGE LABEL – PRINCIPAL DISPLAY – Xylocaine - MPF 20 mL Ampule Label
NDC 63323-493-91
491391
Xylocaine® - MPF (lidocaine HCl Injection, USP)
1.5% (15 mg/mL)
Not For Inhalation.
20 mL ampule
Rx only
PACKAGE LABEL – PRINCIPAL DISPLAY – Xylocaine - MPF 20 mL Ampule Lidding Label
NDC 63323-493-91
491391
Xylocaine® - MPF (lidocaine HCl Injection, USP)
1.5% (15 mg/mL)
For Infiltration and Nerve Block Including Caudal and Epidural Use.
Not For Inhalation.
Methylparaben Free
Rx only

PACKAGE LABEL – PRINCIPAL DISPLAY – Xylocaine - MPF 20 mL Ampule Carton Panel
NDC 63323-493-91
491391
Xylocaine® - MPF (lidocaine HCl Injection, USP)
1.5% (15 mg/mL)
For Infiltration and Nerve Block Including Caudal and Epidural Use.
Not For Inhalation.
Methylparaben Free
Rx only
Sterile-Pak
Contains Five Presterilized
20 mL Plastic Ampule Units

PACKAGE LABEL – PRINCIPAL DISPLAY – Xylocaine - MPF 10 mL Ampule Label
NDC 63323-496-97
491697
Xylocaine® - MPF (lidocaine HCl Injection, USP)
2% (20 mg/mL)
Not For Inhalation.
10 mL ampule
Rx only

PACKAGE LABEL – PRINCIPAL DISPLAY – Xylocaine - MPF 10 mL Ampule Lidding Label
NDC 63323-496-97
491697
Xylocaine® - MPF (lidocaine HCl Injection, USP)
2% (20 mg/mL)
For Infiltration and Nerve Block Including Caudal and Epidural Use.
Not For Inhalation.
Methylparaben Free
Rx only

PACKAGE LABEL – PRINCIPAL DISPLAY – Xylocaine – MPF 10 mL Ampule Carton Panel
NDC 63323-496-97
491697
Xylocaine® - MPF (lidocaine HCl Injection, USP)
2% (20 mg/mL)
For Infiltration and Nerve Block Including Caudal and Epidural Use.
Not For Inhalation.
Methylparaben Free
Rx only
Sterile-Pak
Contains Five Presterilized
10 mL Plastic Ampule Units

|