|
新的吸入性炭疽治疗药物Anthim (obiltoxaximab)获美国FDA批准
There have been no studies of the safety or PK of ANTHIM conducted in the pediatric population. The dosing recommendations in Table 1 are derived from simulations using a population PK approach designed to match the observed adult exposure to ANTHIM at a 16 mg/kg dose [see Use in Specific Populations (8.4)]. 2.3 Preparation and Dilution for Administration Important Preparation Instructions Keep vials in their cartons prior to preparation of an infusion solution to protect ANTHIM from light. ANTHIM vials contain no preservative. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Discard the vial if the solution is discolored or contains extraneous particles other than a few translucent-to- white, proteinaceous particles [see Description (11)]. Do not shake the vial. Table 2. ANTHIM Dose, Total Infusion Volume and Infusion Rate by Body Weight
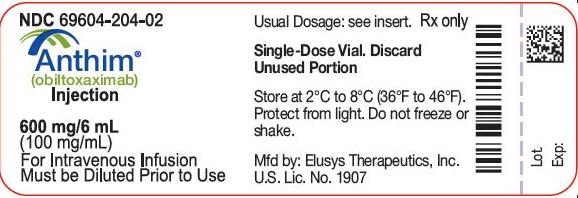
Preparation and Dilution in Bag for Infusion Calculate the milligrams of ANTHIM injection needed by multiplying the recommended mg/kg dose in Table 2 by the patient weight in kilograms. Calculate the required volume in milliliters of ANTHIM injection and number of vials needed for the dose by dividing the calculated dose in milligrams (step 1) by the concentration, 100 mg/mL. Each single vial allows delivery of 6 mL of ANTHIM. Select an appropriate size bag of 0.9% Sodium Chloride Injection, USP. Withdraw a volume of solution from the bag equal to the calculated volume in milliliters of ANTHIM in step 2 above. Discard the solution that was withdrawn from the bag. Withdraw the required volume of ANTHIM injection (calculated from step 2) from the ANTHIM vial(s). Discard any unused portion remaining in the ANTHIM vial(s). Transfer the required volume of ANTHIM injection to the selected infusion bag. Gently invert the bag to mix the solution. Do not shake. The prepared solution is stable for 4 hours stored at room temperature or 4 hours stored in the refrigerator at 2°C to 8°C (36°F to 46°F). Preparation and Dilution in Syringe for Infusion Calculate the milligrams of ANTHIM injection needed by multiplying the recommended mg/kg dose in Table 2 by the patient weight in kilograms. Calculate the required volume in milliliters of ANTHIM injection and number of vials needed for the dose by dividing the calculated dose in milligrams (step 1) by the concentration, 100 mg/mL. Each single vial allows delivery of 6 mL of ANTHIM. Select an appropriate size syringe for the total volume of infusion to be administered. Using the selected syringe, withdraw the required volume of ANTHIM injection (calculated from step 2). Discard any unused portion remaining in the ANTHIM vial(s). Withdraw an appropriate amount of 0.9% Sodium Chloride Injection, USP to prepare the total infusion volume specified in Table 2. Gently mix the solution. Do not shake. Once a diluted solution of ANTHIM has been prepared, administer immediately. Do not store solution in syringe. Discard unused product. 2.4 Administration Administer ANTHIM in appropriately monitored settings which are equipped to manage anaphylaxis [see Warnings and Precautions (5.1)]. Dilute ANTHIM injection [see Dosage and Administration (2.3)] before administering ANTHIM intravenously using the bag or syringe for infusion. After preparation of the bag or syringe for infusion administer the infusion solution using a 0.22 micron inline filter with the infusion rate described in Table 2 [see Dosage and Administration (2.3)]. Administer diluted ANTHIM intravenous infusion over 1 hour and 30 minutes. Monitor patients closely for signs and symptoms of hypersensitivity throughout the infusion and for a period of time after administration [see Warnings and Precautions (5.1)]. Stop the infusion immediately and treat appropriately, if hypersensitivity or anaphylaxis occurs [see Warnings and Precautions (5.1)]. Flush the line with 0.9% Sodium Chloride Injection, USP at the end of the intravenous infusion. 3 DOSAGE FORMS AND STRENGTHS Injection: 600 mg/6 mL (100 mg/mL) in a single-dose vial. ANTHIM is a clear to opalescent, colorless to pale yellow to pale brownish-yellow solution and may contain few translucent-to-white proteinaceous particulates. 4 CONTRAINDICATIONS None. 5 WARNINGS AND PRECAUTIONS 5.1 Hypersensitivity and Anaphylaxis Hypersensitivity reactions were the most common adverse reactions in the safety trials of ANTHIM, occurring in 34/320 healthy subjects (10.6%). Three (0.9%) cases of anaphylaxis occurred during or immediately after the infusion. In clinical trials, manifestations of anaphylaxis were rash/urticaria, cough, dyspnea, cyanosis, postural dizziness and chest discomfort. ANTHIM infusion was discontinued in 8 (2.5%) subjects due to hypersensitivity or anaphylaxis. The adverse reactions reported in these 8 subjects included urticaria, rash, cough, pruritus, dizziness, throat irritation, dysphonia, dyspnea and chest discomfort. The remaining subjects with hypersensitivity had predominantly skin-related symptoms such as pruritus and rash, and 6 subjects reported cough [see Adverse Reactions 6.1]. Due to the risk of anaphylaxis, ANTHIM should be administered in monitored settings by personnel trained and equipped to manage anaphylaxis. Patients should be monitored closely throughout the infusion period and for a period of time after administration [see Patient Counseling Information (17)]. If anaphylaxis or hypersensitivity reactions occur, stop the infusion immediately and treat appropriately. Premedication with diphenhydramine is recommended prior to administration of ANTHIM [see Dosage and Administration (2.1) and Adverse Reactions (6.1)]. Diphenhydramine premedication does not prevent anaphylaxis, and may mask or delay onset of symptoms of hypersensitivity. 6 ADVERSE REACTIONS The following clinically important adverse reactions are described elsewhere in the labeling: Hypersensitivity and Anaphylaxis [see Warnings and Precautions (5.1)]. 6.1 Clinical Trial Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The safety of ANTHIM has been studied only in healthy volunteers. It has not been studied in patients with inhalational anthrax. The safety of ANTHIM was evaluated in 320 healthy subjects treated with one or more 16 mg/kg IV doses in three clinical studies. Study 1 was a placebo-controlled study evaluating a single dose of ANTHIM vs. placebo (210 subjects received ANTHIM, 70 received placebo). Study 2 was a repeat-dose study in which 70 subjects received the first dose, but 34 and 31 subjects received a second dose of ANTHIM in sequences A (2 weeks apart) and B (≥ 4 months apart), respectively. Study 3 was a drug interaction study of a single dose of ANTHIM with ciprofloxacin in 40 subjects (20 subjects received ANTHIM alone and 20 subjects received ANTHIM plus ciprofloxacin for 9 days). Subjects were 18 to 79 years of age, 54% were male, 70% Caucasian, 26% Black/African American, 2% American Indian/Alaska Native, 1% Asian and 10% Hispanic. Adverse Reactions Leading to Discontinuation of ANTHIM Infusion ANTHIM infusion was discontinued in 8/320 healthy subjects (2.5%) in clinical trials due to hypersensitivity reactions or anaphylaxis [see Warnings and Precautions (5.1)]. Most Frequently Reported Adverse Reactions The most frequently reported adverse reactions were headache, pruritus, infections of the upper respiratory tract, cough, vessel puncture site bruise, infusion site swelling, urticaria, nasal congestion, infusion site pain, and pain in extremity. Table 3 shows the adverse reactions that occurred in ≥1.5% of healthy subjects receiving a single dose of ANTHIM (16 mg/kg IV) and more frequently than those receiving placebo. Table 3. Adverse Reactions Reported in ≥ 1.5% of Healthy Adult Subjects Exposed to a Single Dose of ANTHIM 16 mg/kg IV
Effect of Diphenhydramine on the Incidence of Adverse Reactions Overall in the single-dose population, subjects who received pre-medication with diphenhydramine were less likely to experience adverse reactions with administration of ANTHIM compared to those who did not (42% vs. 58% respectively). Specifically, the incidence of the following adverse reactions was lower in the subjects who received diphenhydramine prior to ANTHIM infusion compared to those who did not: headache (5% vs. 16%), cough (1% vs. 8%), rash (2% vs. 7%), pruritus (3% vs. 4%) throat irritation (0 vs. 3%), rhinorrhea (0 vs. 3%), and infusion site erythema (0% vs. 4%). Somnolence was only reported in subjects who were pretreated with diphenhydramine. Less Common Adverse Reactions Clinically significant adverse reactions that were reported in <1.5% of subjects exposed to ANTHIM and at rates higher than in placebo subjects are listed below: General disorders and administration site conditions: chest discomfort/pain, fatigue, pyrexia, intravenous site discoloration Musculoskeletal and connective tissue disorders: myalgia, musculoskeletal pain Respiratory, thoracic and mediastinal disorders: oropharyngeal pain, sinus congestion, rhinorrhea, dysphonia, dyspnea Investigations: lymphocyte count decreased, neutrophil count decreased, white blood count decreased, increased creatine phosphokinase Cardiac disorders: palpitations, cyanosis Neurologic disorders: dizziness Gastrointestinal disorders: vomiting, dry mouth 6.2 Immunogenicity As with all therapeutic proteins, there is a potential for immunogenicity. The development of anti-ANTHIM antibodies was evaluated in all subjects receiving single and double doses of ANTHIM in studies 1, 2 and 3. Eight subjects (2.5%) who received at least one dose of IV ANTHIM were positive for a treatment-emergent anti-therapeutic antibody (ATA) response. Quantitative titers were low ranging from 1:20 – 1:320. There was no evidence of altered PK or toxicity profile in subjects with ATA development. The incidence of antibody formation is highly dependent on the sensitivity and specificity of the immunogenicity assay. Additionally, the observed incidence of any antibody positivity in an assay is highly dependent on several factors, including assay sensitivity and specificity, assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of incidence of antibodies to obiltoxaximab with the incidence of antibodies to other products may be misleading. 7 DRUG INTERACTIONS 7.1 Ciprofloxacin Co-administration of 16 mg/kg ANTHIM intravenously with intravenous or oral ciprofloxacin in human subjects did not alter the PK of either ciprofloxacin or obiltoxaximab [see Clinical Pharmacology (12.3)]. 8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Pregnancy Category B No adequate and well-controlled studies in pregnant women were conducted. Because animal reproduction studies are not always predictive of human response, ANTHIM should be used during pregnancy only if clearly needed. A single embryonic-fetal development study was conducted in pregnant, healthy New Zealand White (NZW) rabbits administered 4 intravenous doses of ANTHIM up to 32 mg/kg (2 times the human dose on a mg/kg basis) on gestation days 6, 10, 13, and 17. No evidence of harm to the pregnant dam or the fetuses due to ANTHIM was observed. Cumulative exposures in NZW rabbits (10,000 mcg•day/mL) at the NOAEL of 32 mg/kg/dose (n=4 doses) based on AUC0-15 days were approximately two-fold the human male and female combined mean AUC at the clinical intravenous dose of 16 mg/kg. Cmax values following a 32 mg/kg/dose were 1180 mcg•day/mL. 8.3 Nursing Mothers ANTHIM has not been evaluated in nursing women. Although human immunoglobulins are excreted in human milk, published data suggest that neonatal consumption of human milk does not result in substantial absorption of these maternal immunoglobulins into circulation. Inform a nursing woman that the effects of local gastrointestinal and systemic exposure to ANTHIM on nursing infant are unknown. 8.4 Pediatric Use As in adults, the effectiveness of ANTHIM in pediatric patients is based solely on efficacy studies in animal models of inhalational anthrax. As exposure of healthy children to ANTHIM is not ethical, a population PK approach was used to derive intravenous dosing regimens that are predicted to provide pediatric patients with exposure comparable to the observed exposure in adults receiving 16 mg/kg. The dose for pediatric patients is based on weight [see Dosage and Administration (2.2)]. There have been no studies of safety or PK of ANTHIM in the pediatric population. 8.5 Geriatric Use Clinical studies of ANTHIM did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects. Of the 320 subjects in clinical studies of ANTHIM, 9.4% (30/320) were 65 years and over, while 2% (6/320) were 75 years and over. No alteration of dosing is needed for patients ≥65 years of age [see Clinical Pharmacology (12.3)]. 10 OVERDOSAGE There is no clinical experience with overdosage of ANTHIM. In case of overdosage, monitor patients for any signs or symptoms of adverse effects. 11 DESCRIPTION Obiltoxaximab is a chimeric IgG1 kappa monoclonal antibody (mAb) that binds the PA component of B. anthracis toxin. It has an approximate molecular weight of 148 kDa. ANTHIM injection is a sterile, preservative-free, clear to opalescent, colorless to pale yellow to pale brownish-yellow solution that may contain few translucent-to-white proteinaceous particulates. ANTHIM is supplied as 600 mg/6 mL in single-dose vials for intravenous infusion. Each mL contains 100 mg obiltoxaximab in L-histidine (6.2 mg), polysorbate 80 (0.1 mg), sorbitol (36 mg) with a pH of 5.5. 12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Obiltoxaximab is a monoclonal antibody that binds the PA of B. anthracis[see Microbiology (12.4)]. 12.3 Pharmacokinetics The PK of obiltoxaximab are linear over the dose range of 4 mg/kg (0.25 times the lowest recommended dose) to 16 mg/kg following single IV administration in healthy subjects. Following single IV administration of ANTHIM 16 mg/kg in healthy, male and female human subjects, the mean Cmax and AUCinf were 400 ± 91.2 mcg/mL and 5170 ± 1360 mcg•day/mL, respectively. Repeat Dosing Although ANTHIM is intended for single dose administration, the PK of obiltoxaximab following a second dose administration of 16 mg/kg IV given 2 weeks or ≥ 4 months after the first 16 mg/kg IV dose was assessed in 65 healthy subjects (study 2). The obiltoxaximab AUCinf following two 16 mg/kg doses 2 weeks apart was approximately twice that after a single 16 mg/kg dose on Day 1 or Day 120. No significant differences in mean estimates of Cmax, AUCinf, CL, or half-life of obiltoxaximab between the 2 doses administered ≥4 months apart were observed. Distribution Mean obiltoxaximab steady-state volume of distribution was greater than plasma volume, suggesting some tissue distribution. Elimination Clearance values were much smaller than the glomerular filtration rate, indicating that there is virtually no renal clearance of obiltoxaximab. Because the effectiveness of ANTHIM cannot be evaluated in humans, a comparison of ANTHIM exposures achieved in healthy human subjects to those observed in animal models of inhalational anthrax in therapeutic efficacy studies is necessary to support the dosage regimen of 16 mg/kg IV as a single dose for the treatment of inhalational anthrax in humans. Based on observed and simulated data, humans achieve similar obiltoxaximab Cmax and greater AUCinf following a single 16 mg/kg IV dose compared to exposures achieved in NZW rabbits and cynomolgus macaques. Specific Populations Gender, Age, and Race ANTHIM PK were evaluated via a population PK analysis using serum samples from 303 healthy adult subjects who received a single IV dose across 3 clinical trials. Based on this analysis, gender (female versus male), race (non-Caucasian versus Caucasian), or age (elderly versus young) had no meaningful effects on the PK parameters for ANTHIM. Pediatric Population ANTHIM PK have not been evaluated in children [see Dosage and Administration (2.2) and Use in Specific Populations (8.4)]. Drug Interaction Studies Ciprofloxacin In an open-label study evaluating the effect of ciprofloxacin on obiltoxaximab PK in healthy adult male and female subjects (study 3), the administration of 16 mg/kg ANTHIM IV infusion prior to ciprofloxacin IV infusion or ciprofloxacin oral tablets twice daily did not alter the PK of obiltoxaximab. Likewise, obiltoxaximab did not alter the PK of ciprofloxacin administered orally and/or intravenously [see Drug Interactions (7.1)]. 12.4 Microbiology Mechanism of Action Obiltoxaximab is a monoclonal antibody that binds free PA with an affinity equilibrium dissociation constant (Kd) of 0.33 nM. Obiltoxaximab inhibits the binding of PA to its cellular receptors, preventing the intracellular entry of the anthrax lethal factor and edema factor, the enzymatic toxin components responsible for the pathogenic effects of anthrax toxin. Activity In Vitro and In Vivo Obiltoxaximab binds in vitro to PA from the Ames, Vollum, and Sterne strains of B. anthracis. Obiltoxaximab binds to an epitope on PA that is conserved across reported strains of B. anthracis. In vitro studies in a cell-based assay, using murine macrophages, suggest that obiltoxaximab neutralizes the toxic effects of lethal toxin, a combination of PA + lethal factor. In vivo efficacy studies in NZW rabbits and cynomolgus macaques challenged with the spores of the Ames strain of B. anthracis by the inhalational route, showed a dose-dependent increase in survival following treatment with ANTHIM. Exposure to B. anthracis spores resulted in increasing concentrations of PA in the serum of NZW rabbits and cynomolgus macaques. After treatment with ANTHIM there was a decrease in PA concentrations in a majority of surviving animals. PA concentrations in placebo animals increased until they died [see Clinical Studies (14)]. 13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenicity, genotoxicity, and fertility studies have not been conducted with obiltoxaximab. 13.2 Animal Toxicology and/or Pharmacology Central nervous system (CNS) lesions (bacteria, inflammation, hemorrhage and occasionally necrosis) were seen in anthrax-infected non-surviving NZW rabbits and cynomolgus macaques administered IV obiltoxaximab (≥4 mg/kg) or control at the time of disease confirmation. Microscopic changes in the non-surviving animals that received obiltoxaximab were due to the presence of extravascular bacteria and not the effect of obiltoxaximab. No dose response relationship for brain histopathology was identified. No treatment-related brain lesions were shown in anthrax-infected surviving NZW rabbits (at day 28) or cynomolgus macaques (up to day 56) after a single administration of obiltoxaximab at doses up to 16 mg/kg and up to 32 mg/kg/dose, respectively. No obiltoxaximab-related neurobehavioral effects were observed in surviving anthrax-infected cynomolgus macaques following treatment with obiltoxaximab. 14 CLINICAL STUDIES Overview Because it is not feasible or ethical to conduct controlled clinical trials in humans with inhalational anthrax, the efficacy of ANTHIM for the treatment of inhalational anthrax is based on efficacy studies in NZW rabbits and cynomolgus macaques. The animal efficacy studies are conducted under widely varying conditions, such that the survival rates observed in the animal studies cannot be directly compared between studies and may not reflect the rates observed in clinical practice. Types of Studies The efficacy of ANTHIM for treatment and prophylaxis of inhalational anthrax was studied in multiple studies in the cynomolgus macaque and NZW rabbit models of inhalational anthrax. These studies tested the efficacy of ANTHIM compared to placebo and the efficacy of ANTHIM in combination with antibacterial drugs relative to the antibacterial drugs alone. Study Design The animals were challenged with aerosolized B. anthracis spores (Ames strain) at approximately 200xLD50 to achieve 100% mortality if untreated. In prophylaxis studies of inhalational anthrax, animals were treated prior to the development of symptoms. In treatment studies, animals were administered treatment after exhibiting clinical signs or symptoms of systemic anthrax. Cynomolgus macaques were treated at the time of a positive serum electrochemiluminescence (ECL) assay for B. anthracis PA at a mean time of approximately 40 hours post-challenge with B. anthracis. In NZW rabbit treatment studies, animals were treated after a positive ECL assay for PA or sustained elevation of body temperature above baseline, at a mean time of approximately 30 hours post-challenge; the majority of animals triggered by temperature. In some of the treatment studies assessing the effect of ANTHIM in combination with antibacterial drugs, treatment was delayed to 72 to 96 hours post-challenge. Most study animals were bacteremic and had a positive ECL assay for PA prior to treatment. Survival was assessed at 28 days post-challenge with B. anthracis in most studies. Results NZW rabbit studies 1 and 2 and cynomolgus macaque studies 3 and 4 evaluated treatment with ANTHIM 16 mg/kg IV single dose compared to placebo in animals with systemic anthrax. Treatment with ANTHIM alone resulted in statistically significant improvement in survival relative to placebo (Table 4). Table 4. Survival Proportions in Monotherapy Treatment Studies of 16 mg/kg IV, All Randomized Animals Positive for Bacteremia Prior to Treatment
1Survival assessed 28 days after spore challenge 2p-value is from 1-sided Boschloo Test (with Berger-Boos modification of gamma=0.001) compared to placebo 3Exact 95% confidence interval of difference in survival rates 4ANTHIM products manufactured at two different facilities were tested in two separate treatment arms ANTHIM administered in combination with antibacterial drugs (levofloxacin, ciprofloxacin and doxycycline) for the treatment of systemic inhalational anthrax disease resulted in higher survival outcomes than antibacterial therapy alone in multiple studies where ANTHIM and antibacterial therapy was given at various doses and treatment times. ANTHIM administered as prophylaxis resulted in higher survival outcomes compared to placebo in multiple studies where treatment was given at various doses and treatment times. In one study, cynomolgus macaques were administered ANTHIM 16 mg/kg at 18 hours, 24 hours or 36 hours after exposure. Survival was 6/6 (100%) at 18 hours, 5/6 (83%) at 24 hours, and 3/6 (50%) at 36 hours. Another cynomolgus macaque study evaluated ANTHIM 16 mg/kg administered 72, 48 or 24 hours prior to exposure. Survival was 100% at all three time points (14/14, 14/14, 15/15, respectively) at day 56 (end of study). 16 HOW SUPPLIED/STORAGE AND HANDLING ANTHIM injection is a sterile, preservative-free, clear to opalescent, colorless to pale yellow to pale brownish-yellow solution that may contain few translucent-to-white proteinaceous particulates in single-dose vials containing 600 mg/6 mL (100 mg/mL) and is available in the following packaging configuration: Carton: Contains one (1) single-dose vial of ANTHIM 600 mg/6 mL (NDC 69604-204-02). Store in refrigerator at 2°C to 8°C (36°F to 46°F) in original carton to protect from light. Do Not Freeze. Do Not Shake.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||