| 2012年11月20日,武田药品在欧盟推出抗体偶联药物Adcetris(brentuximab vedotin),该药是近30多年来首个获批用于复发性或难治性CD30阳性霍奇金淋巴瘤的靶向性治疗药物,用于2种适应症:(1)既往经自体干细胞移植(AST)治疗,或既往已接受至少2种疗法而AST或多药化疗不能作为治疗方案的复发性或难治性CD30阳性霍奇金淋巴瘤(HL)成人患者;(2)复发性或难治性系统性间变性大细胞淋巴瘤(sALCL)成人患者。 Adcetris由武田及美国西雅图遗传学公司(Seattle Genetics)联合开发,该药已于2011年8月获得了FDA的批准,并于上月获得了欧盟委员会(EC)授予的有条件上市许可(conditional Marketing Authorisation)。欧盟委员会授予的有条件上市许可,意味着制药公司有特定的义务,在后期的大型临床试验提供更多的临床数据,以确认该药积极的利益-风险平衡(positive benefit-risk balance)。 临床试验中,ADCETRIS已被证明能够在这2种适应症中,提供较高的总体反应率及持续完整响应。对于CD30阳性复发性或难治性霍奇金淋巴瘤患者来说,欧盟委员会对于Adcetris的有条件上市许可批准,标志着该患者群体临床治疗的重大进步。 Adcetris是一种抗体偶联药物(ADC),靶向于CD30,该蛋白是经典HL及sALCL的明确标志物。 Adcetris最常见的副作用有:减少起对抗感染作用的白血细胞(嗜中性白血球减少症),神经损伤(周围感觉神经病变),疲劳,恶心,贫血,上呼吸道感染,腹泻,发烧,咳嗽,呕吐,和血小板水平低下(血小板减少症)。此外,孕妇应注意ADCETRIS可能对未出生的婴儿造成损害 Adcetris 50 mg powder for concentrate for solution for infusion 1. Name of the medicinal product ADCETRIS 50 mg powder for concentrate for solution for infusion. 2. Qualitative and quantitative composition Each vial contains 50 mg of brentuximab vedotin. After reconstitution (see section 6.6), each ml contains 5 mg of brentuximab vedotin. ADCETRIS is an antibody-drug conjugate composed of a CD30-directed monoclonal antibody (recombinant chimeric immunoglobulin G1 [IgG1], produced by recombinant DNA technology in Chinese Hamster ovary cells) that is covalently linked to the antimicrotubule agent monomethyl auristatin E (MMAE). Excipients with known effect Each vial contains approximately 13.2 mg of sodium. For the full list of excipients, see section 6.1. 3. Pharmaceutical form Powder for concentrate for solution for infusion. White to off-white cake or powder. 4. Clinical particulars 4.1 Therapeutic indications ADCETRIS is indicated for the treatment of adult patients with relapsed or refractory CD30+ Hodgkin lymphoma (HL): 1. following autologous stem cell transplant (ASCT) or 2. following at least two prior therapies when ASCT or multi-agent chemotherapy is not a treatment option. ADCETRIS is indicated for the treatment of adult patients with relapsed or refractory systemic anaplastic large cell lymphoma (sALCL). 4.2 Posology and method of administration Brentuximab vedotin should be administered under the supervision of a physician experienced in the use of anti-cancer agents. Posology The recommended dose is 1.8 mg/kg administered as an intravenous infusion over 30 minutes every 3 weeks. Renal impairment The recommended starting dose in patients with severe renal impairment is 1.2 mg/kg administered as an intravenous infusion over 30 minutes every 3 weeks. Patients with renal impairment should be closely monitored for adverse events (see section 5.2). Hepatic impairment The recommended starting dose in patients with hepatic impairment is 1.2 mg/kg administered as an intravenous infusion over 30 minutes every 3 weeks. Patients with hepatic impairment should be closely monitored for adverse events (see section 5.2). If the patient's weight is more than 100 kg, the dose calculation should use 100 kg (see section 6.6). Complete blood counts should be monitored prior to administration of each dose of this treatment (see section 4.4). Patients should be monitored during and after infusion (see section 4.4). Treatment should be continued until disease progression or unacceptable toxicity (see section 4.4). Patients who achieve stable disease or better should receive a minimum of 8 cycles and up to a maximum of 16 cycles (approximately 1 year) (see section 5.1). Dose adjustments Neutropenia If neutropenia develops during treatment it should be managed by dose delays. See Table 1 below for appropriate dosing recommendations (see also section 4.4). Table 1: Dosing recommendations for neutropenia
b. Patients who develop Grade 3 or Grade 4 lymphopenia may continue treatment without interruption. Peripheral neuropathy If peripheral sensory or motor neuropathy emerges or worsens during treatment see Table 2 below for appropriate dosing recommendations (see section 4.4). Table 2: Dosing recommendations for new or worsening peripheral sensory or motor neuropathy
Older patients The safety and efficacy in older patients aged 65 and older have not been established. No data are available. Paediatric population The safety and efficacy of children less than 18 years have not yet been established. No data are available. In nonclinical studies, thymus depletion has been observed (see section 5.3). Method of administration The recommended dose of ADCETRIS is infused over 30 minutes. For instructions on reconstitution and dilution of the medicinal product before administration, see section 6.6. Brentuximab vedotin must not be administered as an intravenous push or bolus. Brentuximab vedotin should be administered through a dedicated intravenous line and it must not be mixed with other medicinal products (see section 6.2). 4.3 Contraindications Hypersensitivity to the active substance or to any of the excipients listed in section 6.1. Combined use of bleomycin and brentuximab vedotin causes pulmonary toxicity. 4.4 Special warnings and precautions for use Progressive multifocal leukoencephalopathy John Cunningham virus (JCV) reactivation resulting in progressive multifocal leukoencephalopathy (PML) and death can occur in brentuximab vedotin-treated patients. PML has been reported in patients who received this treatment after receiving multiple prior chemotherapy regimens. PML is a rare demyelinating disease of the central nervous system that results from reactivation of latent JCV and is often fatal. Patients should be closely monitored for new or worsening neurological, cognitive, or behavioural signs or symptoms, which may be suggestive of PML. Brentuximab vedotin dosing should be held for any suspected case of PML. Suggested evaluation of PML includes neurology consultation, gadolinium-enhanced magnetic resonance imaging of the brain and cerebrospinal fluid analysis for JCV DNA by polymerase chain reaction or a brain biopsy with evidence of JCV. A negative JCV PCR does not exclude PML. Additional follow up and evaluation may be warranted if no alternative diagnosis can be established. Brentuximab vedotin dosing should be permanently discontinued if a diagnosis of PML is confirmed. The physician should be particularly alert to symptoms suggestive of PML that the patient may not notice (e.g., cognitive, neurological, or psychiatric symptoms). Pancreatitis Acute pancreatitis has been observed in patients treated with brentuximab vedotin. Fatal outcomes have been reported. Patients should be closely monitored for new or worsening abdominal pain, which may be suggestive of acute pancreatitis. Patient evaluation may include physical examination, laboratory evaluation for serum amylase and serum lipase, and abdominal imaging, such as ultrasound and other appropriate diagnostic measures. Brentuximab vedotin should be held for any suspected case of acute pancreatitis. Brentuximab vedotin should be discontinued if a diagnosis of acute pancreatitis is confirmed. Pulmonary Toxicity Cases of pulmonary toxicity have been reported in patients receiving brentuximab vedotin. Although a causal association with brentuximab vedotin has not been established, the risk of pulmonary toxicity cannot be ruled out. In the event of new or worsening pulmonary symptoms (e.g., cough, dyspnoea), a prompt diagnostic evaluation should be performed and patients should be treated appropriately. Serious infections and opportunistic infections Serious infections such as pneumonia, staphylococcal bacteraemia, sepsis/septic shock (including fatal outcomes) and herpes zoster, and opportunistic infections such as Pneumocystis jiroveci pneumonia and oral candidiasis have been reported in patients treated with brentuximab vedotin. Patients should be carefully monitored during treatment for the emergence of possible serious and opportunistic infections. Infusion-related reactions Immediate and delayed infusion-related reactions (IRR), as well as anaphylactic reactions, have been reported. Patients should be carefully monitored during and after infusion. If an anaphylactic reaction occurs, administration of brentuximab vedotin should be immediately and permanently discontinued and appropriate medical therapy should be administered. If an infusion-related reaction occurs, the infusion should be interrupted and appropriate medical management instituted. The infusion may be restarted at a slower rate after symptom resolution. Patients who have experienced a prior infusion-related reaction should be premedicated for subsequent infusions. Premedication may include paracetamol, an antihistamine and a corticosteroid. Infusion-related reactions are more frequent and more severe in patients with antibodies to brentuximab vedotin (see section 4.8). Tumour lysis syndrome Tumour lysis syndrome (TLS) has been reported with brentuximab vedotin. Patients with rapidly proliferating tumour and high tumour burden are at risk of tumour lysis syndrome. These patients should be monitored closely and managed according to best medical practice. Management of TLS may include aggressive hydration, monitoring of renal function, correction of electrolyte abnormalities, anti-hyperuricaemic therapy, and supportive care. Peripheral neuropathy Brentuximab vedotin treatment may cause a peripheral neuropathy that is predominantly sensory. Cases of peripheral motor neuropathy have also been reported. Brentuximab vedotin-induced peripheral neuropathy is typically an effect of cumulative exposure to this medicinal product and is reversible in most cases. In the phase 2 population, at the time of last evaluation, the majority of patients (62%) had improvement or resolution of their peripheral neuropathy symptoms. For patients who reported peripheral neuropathy, brentuximab vedotin treatment discontinuation occurred in 9%, dose reductions were reported in 8%, and dose delays occurred in 13% of patients. Patients should be monitored for symptoms of neuropathy, such as hypoesthesia, hyperesthesia, paraesthesia, discomfort, a burning sensation, neuropathic pain or weakness. Patients experiencing new or worsening peripheral neuropathy may require a delay and a dose reduction of brentuximab vedotin or discontinuation of treatment (see section 4.2). Haematological toxicities Grade 3 or Grade 4 anaemia, thrombocytopenia, and prolonged (≥1 week) Grade 3 or Grade 4 neutropenia can occur with brentuximab vedotin. Complete blood counts should be monitored prior to administration of each dose. If Grade 3 or Grade 4 neutropenia develops, refer to section 4.2. Febrile neutropenia Febrile neutropenia (fever of unknown origin without clinically or microbiologically documented infection with an absolute neutrophil count <1.0 x 109/L, fever ≥38.5°C; ref CTCAE v3) has been reported with treatment with brentuximab vedotin. Complete blood counts should be monitored prior to administration of each dose of this treatment. Patients should be monitored closely for fever and managed according to best medical practice if febrile neutropenia develops. Stevens-Johnson syndrome and toxic epidermal necrolysis Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have been reported with brentuximab vedotin. Fatal outcomes have been reported. If SJS or TEN occur, treatment with brentuximab vedotin should be discontinued and appropriate medical therapy should be administered. Hepatic function Elevations in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) have been reported. Liver function should be routinely monitored in patients receiving brentuximab vedotin. Hyperglycaemia Hyperglycaemia has been reported during clinical trials in patients with an elevated Body Mass Index (BMI) with or without a history of diabetes mellitus. However, any patient who experiences an event of hyperglycaemia should have their serum glucose closely monitored. Anti-diabetic treatment should be administered as appropriate. Renal and hepatic impairment There is limited experience in patients with renal and hepatic impairment. Available data indicate that MMAE clearance might be affected by severe renal impairment, hepatic impairment, and by low serum albumin concentrations (see section 5.2). Sodium content in excipients This medicinal product contains a maximum of 2.1 mmol (or 47 mg) of sodium per dose. To be taken into consideration for patients on a controlled sodium diet. 4.5 Interaction with other medicinal products and other forms of interaction Interaction with medicinal products metabolized through CYP3A4 route (CYP3A4 inhibitors/inducers) Co-administration of brentuximab vedotin with ketoconazole, a strong CYP3A4 and P-gp inhibitor, increased the exposure to the antimicrotubule agent MMAE by approximately 73%, and did not alter the plasma exposure to brentuximab vedotin. Therefore, co-administration of brentuximab vedotin with strong CYP3A4 and P-gp inhibitors may increase the incidence of neutropenia. If neutropenia develops, refer to Table 1: Dosing recommendations for neutropenia (see section 4.2). Co-administration of brentuximab vedotin with rifampicin, a strong CYP3A4 inducer, did not alter the plasma exposure to brentuximab vedotin; however it reduced exposure to MMAE by approximately 31%. Co-administration of midazolam, a CYP3A4 substrate, with brentuximab vedotin did not alter the metabolism of midazolam; therefore brentuximab vedotin is not expected to alter the exposure to medicines that are metabolized by CYP3A4 enzymes. 4.6 Fertility, pregnancy and lactation Women of childbearing potential Women of childbearing potential should be using two methods of effective contraception during treatment with brentuximab vedotin and until 6 months after treatment. Pregnancy There are no data from the use of brentuximab vedotin in pregnant women. Studies in animals have shown reproductive toxicity (see section 5.3). Brentuximab vedotin should not be used during pregnancy unless the benefit to the mother outweighs the potential risks to the foetus. If a pregnant woman needs to be treated she should be clearly advised on the potential risk to the foetus. See the fertility section below pertaining to advice for women whose male partners are being treated with brentuximab vedotin. Breastfeeding There are no data as to whether brentuximab vedotin or its metabolites are excreted in human milk. A risk to the newborn/infant cannot be excluded. A decision should be made whether to discontinue breast-feeding or to discontinue/abstain from this therapy, taking into account a potential risk of breast-feeding for the child and the benefit of therapy for the woman. Fertility In non-clinical studies, brentuximab vedotin treatment has resulted in testicular toxicity, and may alter male fertility. MMAE has been shown to have aneugenic properties (see section 5.3). Therefore, men being treated with this medicine are advised to have sperm samples frozen and stored before treatment. Men being treated with this medicine are advised not to father a child during treatment and for up to 6 months following the last dose. 4.7 Effects on ability to drive and use machines Brentuximab vedotin may have a minor influence on the ability to drive and use machines. 4.8 Undesirable effects Summary of the safety profile The safety profile of ADCETRIS is based on available clinical trial data, the Named Patient Program (NPP), and post-marketing experience to date. Frequencies of adverse reactions described below and in Table 3 have been determined based on data generated from clinical studies. Serious infections and opportunistic infections have been reported in patients treated with this medicine (see section 4.4). In the phase 2 population, 16% of patients reported an event term that referred to an infection. Serious adverse drug reactions in the phase 2 population were: neutropenia, thrombocytopenia, constipation, diarrhoea, vomiting, pyrexia, peripheral motor neuropathy and peripheral sensory neuropathy, hyperglycaemia, demyelinating polyneuropathy, tumour lysis syndrome and Stevens-Johnson syndrome. The most frequently observed adverse reactions in the phase 2 population were: peripheral sensory neuropathy, fatigue, nausea, diarrhoea, neutropenia, vomiting, pyrexia, and upper respiratory tract infection. In the phase 2 population, adverse reactions led to treatment discontinuation in 19% of patients receiving brentuximab vedotin. Serious adverse reactions that led to treatment discontinuation in two or more HL or sALCL patients were peripheral sensory neuropathy (6%) and peripheral motor neuropathy (2%). The safety data in patients with relapsed or refractory HL who had not received an autologous stem cell transplant and were treated with the recommended dose of 1.8 mg/kg every three weeks in the phase 1 dose escalation and clinical pharmacology studies (n=15 patients) and in the NPP (n=26 patients) (see section 5.1) were consistent with the safety profile of the pivotal clinical studies. Tabulated list of adverse reactions Adverse reactions for ADCETRIS are listed by MedDRA System Organ Class and Preferred Term (see Table 3). Within each System Organ Class, adverse reactions are listed under frequency categories of: Very common (≥1/10); Common (≥1/100 to <1/10); Uncommon (≥1/1,000 to <1/100); Rare (≥1/10,000 to <1/1,000); Very rare (<1/10,000); not known (cannot be estimated from the available data). Table 3: Adverse reactions to ADCETRIS
b. Preferred terms associated with infusion-related reactions were chills (4%), nausea, dyspnoea and pruritus (3% each), and cough (2%). Description of selected adverse reactions Adverse reactions that led to dose delays of up to 3 weeks in more than 5% of patients were neutropenia (14%) and peripheral sensory neuropathy (11%) (see section 4.2). The adverse reaction that led to a dose reduction in more than 5% of patients was peripheral sensory neuropathy (8%). Ninety percent (90%) of patients in the phase 2 studies remained at the recommended dose of 1.8 mg/kg while on treatment. Severe and prolonged (≥1 week) neutropenia can occur with this treatment which may increase the risk of patients developing serious infections. The median duration of Grade 3 or Grade 4 neutropenia was limited (1 week); 2% of patients had Grade 4 neutropenia that lasted ≥7 days. Less than half of the patients in the phase 2 population with Grade 3 or Grade 4 neutropenia had temporally associated infections, and the majority of temporally associated infections were Grade 1 or Grade 2. Among patients who experienced peripheral neuropathy, the median follow up time from end of treatment until last evaluation was approximately 10 weeks. At the time of last evaluation, 62% of the 84 patients who experienced peripheral neuropathy had resolution or improvement of their peripheral neuropathy symptoms. The median time from onset to resolution or improvement for all events was 6.6 weeks (range from 0.3 weeks to 54.4 weeks). PML has been reported outside of the pivotal phase 2 clinical trials (see section 4.4). Acute pancreatitis (including fatal outcomes) has been reported outside of the pivotal phase 2 clinical trials. Consider the diagnosis of acute pancreatitis for patients presenting with new or worsening abdominal pain (see section 4.4). Anaphylactic reactions have been reported outside of the pivotal phase 2 clinical trials (see section 4.4). Symptoms of an anaphylactic reaction may include, but are not limited to, urticaria, angioedema, hypotension and bronchospasm. Febrile neutropenia has been reported outside of the pivotal phase 2 clinical trials (see section 4.2). A patient enrolled in a phase 1 dose escalation trial experienced Grade 5 febrile neutropenia after receiving a single dose of 3.6 mg/kg of brentuximab vedotin. Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have been reported with brentuximab vedotin in clinical trials and post-marketing use. Fatal outcomes have been reported (see section 4.4). Immunogenicity Patients with relapsed or refractory HL or sALCL in two phase 2 studies were tested for antibodies to brentuximab vedotin every 3 weeks using a sensitive electrochemiluminescent immunoassay. Approximately 35% of patients in these studies developed antibodies to brentuximab vedotin. Of these patients, the majority became positive prior to dose 2, 7% were persistently anti-therapeutic antibodies (ATA)-positive, and 62% of the ATA-positive patients had neutralizing antibodies. One (1) percent of patients experienced adverse reactions consistent with infusion-related reactions that led to discontinuation of treatment. The presence of antibodies to brentuximab vedotin did not correlate with a clinically meaningful reduction in serum brentuximab vedotin levels and did not result in a decrease in the efficacy of brentuximab vedotin. While the presence of antibodies to brentuximab vedotin does not necessarily predict the development of an IRR, there was a higher incidence of IRRs observed in patients with persistently positive ATA (30%) relative to patients with transiently positive ATA (12%) and never positive ATA (7%). Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the Yellow Card Scheme at: www.mhra.gov.uk/yellowcard. 4.9 Overdose There is no known antidote for overdose of brentuximab vedotin. In case of overdose, the patient should be closely monitored for adverse reactions, particularly neutropenia, and supportive treatment should be administered (see section 4.4). 5. Pharmacological properties 5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents; other antineoplastic agents; monoclonal antibodies, ATC code: L01XC12 Mechanism of action Brentuximab vedotin is an antibody drug conjugate (ADC) that delivers an antineoplastic agent that results in apoptotic cell death selectively in CD30-expressing tumour cells. Nonclinical data suggest that the biological activity of brentuximab vedotin results from a multi-step process. Binding of the ADC to CD30 on the cell surface initiates internalisation of the ADC-CD30 complex, which then traffics to the lysosomal compartment. Within the cell, a single defined active species, MMAE, is released via proteolytic cleavage. Binding of MMAE to tubulin disrupts the microtubule network within the cell, induces cell cycle arrest and results in apoptotic death of the CD30-expressing tumour cell. Classical HL and sALCL express CD30 as an antigen on the surface of their malignant cells. This expression is independent of disease stage, line of therapy or transplant status. These features make CD30 a target for therapeutic intervention. Because of the CD30-targeted mechanism of action brentuximab vedotin is able to overcome chemo-resistance as CD30 is consistently expressed in patients who are refractory to multi-agent chemotherapy, irrespective of prior transplant status. The CD30-targeted mechanism of action of brentuximab vedotin, the consistent expression of CD30 throughout the classical HL and sALCL disease and therapeutic spectrums and clinical evidence in two CD30-positive malignancies following multiple lines of treatment provide a biologic rationale for its use in patients with relapsed and refractory classical HL and sALCL with or without prior ASCT. Contributions to the mechanism of action by other antibody associated functions have not been excluded. Pharmacodynamic effects Cardiac electrophysiology Forty-six (46) patients with CD30-expressing hematologic malignancies were evaluable of the 52 patients who received 1.8 mg/kg of brentuximab vedotin every 3 weeks as part of a phase 1, single-arm, open-label, multicenter cardiac safety study. The primary objective was to evaluate the effect of brentuximab vedotin on cardiac ventricular re-polarization and the predefined primary analysis was the change in QTc from baseline to multiple time points in Cycle 1. The upper 90% confidence interval (CI) around the mean effect on QTc was <10 msec at each of the Cycle 1 and Cycle 3 post-baseline time points. These data indicate the absence of clinically relevant QT prolongation due to brentuximab vedotin administered at a dose of 1.8 mg/kg every 3 weeks in patients with CD30-expressing malignancies. Clinical efficacy Hodgkin lymphoma The efficacy and safety of brentuximab vedotin as a single agent was evaluated in a pivotal open-label, single-arm, multicenter study (study SG035-0003) in 102 patients with relapsed or refractory HL. See Table 4 below for a summary of baseline patient and disease characteristics. Table 4: Summary of baseline patient and disease characteristics in the phase 2 relapsed or refractory HL study
Eighteen (18) patients (18%) received 16 cycles of brentuximab vedotin; and the median number of cycles received was 9 (ranging from 1 to 16). Response to treatment with brentuximab vedotin was assessed by Independent Review Facility (IRF) using the Revised Response Criteria for Malignant Lymphoma (Cheson, 2007). Treatment response was assessed by spiral CT of chest, neck, abdomen and pelvis; PET scans and clinical data. Response assessments were performed at cycles 2, 4, 7, 10, 13, and 16 with PET at cycles 4 and 7. The objective response rate (ORR) per IRF assessment was 75% (76 of 102 patients in the intent-to-treat [ITT] set) and tumour reduction was achieved in 94% of patients. Complete remission (CR) was 33% (34 of 102 patients in the ITT set). The median overall survival (OS) is 40.5 months (the median observation time (time to death or last contact) from first dose was 32.7 months). The investigator assessments were generally consistent with the independent review of the scans. Of the patients treated, 7 responding patients went on to receive an allogeneic SCT. For further efficacy results see Table 5. Table 5: Efficacy results in relapsed or refractory Hodgkin lymphoma patients treated with 1.8 mg/kg of brentuximab vedotin every 3 weeks
b. Not estimable. An exploratory intra-patient analysis showed that approximately 64% of the HL patients treated with brentuximab vedotin as part of the SG035-0003 clinical study experienced an improvement in clinical benefit as measured by longer progression free survival (PFS) compared with their most recent prior line of therapy. Of the 35 patients (33%) who had B symptoms at baseline, 27 patients (77%) experienced resolution of all B symptoms at a median time of 0.7 months from initiation of brentuximab vedotin. Data were collected from patients (n=15) in phase 1 dose escalation and clinical pharmacology studies, and from patients (n=26) in a NPP, with relapsed or refractory HL who had not received an ASCT, and who were treated with 1.8 mg/kg of brentuximab vedotin every 3 weeks. Baseline patient characteristics showed failure from multiple prior chemotherapy regimens (median of 3 with a range of 1 to 7) before first administration with brentuximab vedotin. Fifty nine percent (59%) of patients had advanced stage disease (stage III or IV) at initial diagnosis. Results from these phase 1 studies and from the NPP experience showed, that in patients with relapsed or refractory HL without prior ASCT, clinically meaningful responses can be achieved as evidenced by an investigator-assessed, objective response rate of 54% and a complete remission rate of 22% after a median of 5 cycles of brentuximab vedotin. Systemic anaplastic large cell lymphoma The efficacy and safety of brentuximab vedotin as a single agent was evaluated in an open-label, single-arm, multicenter study (study SG035-0004) in 58 patients with relapsed or refractory sALCL. See Table 6 below for a summary of baseline patient and disease characteristics. Table 6: Summary of baseline patient and disease characteristics in the phase 2 relapsed or refractory sALCL study
b. Primary refractory sALCL is defined as a failure to achieve a complete remission to, or progressed within 3 months of completing frontline therapy. The median time from initial sALCL diagnosis to first dose with brentuximab vedotin was 16.8 months. Ten (10) patients (17%) received 16 cycles of brentuximab vedotin; the median number of cycles received was 7 (range, 1 to 16). Response to treatment with brentuximab vedotin was assessed by Independent Review Facility (IRF) using the Revised Response Criteria for Malignant Lymphoma (Cheson, 2007). Treatment response was assessed by spiral CT of chest, neck, abdomen and pelvis; PET scans and clinical data. Response assessments were performed at cycles 2, 4, 7, 10, 13 and 16 with PET at cycles 4 and 7. The ORR per IRF assessment was 86% (50 of 58 patients in the ITT set). CR was 59% (34 of 58 patients in the ITT set) and tumour reduction was achieved in 97% of patients. The estimated 36 month overall survival was 63% (the median observation time (time to death or last contact) from first dose was 33.4 months). The investigator assessments were generally consistent with the independent review of the scans. Of the patients treated, 9 responding patients went on to receive an allogeneic stem cell transplant (SCT) and 7 responding patients went on to autologous SCT. For further efficacy results, see Table 7. Table 7: Efficacy results in relapsed or refractory sALCL patients treated with 1.8 mg/kg of brentuximab vedotin every 3 weeks
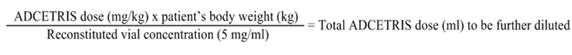
b. Not estimable. c. The estimated 36 month overall survival was 63% (the median observation time (time to death or last contact) from first dose was 33.4 months). An exploratory intra-patient analysis showed that approximately 69% of the sALCL patients treated with brentuximab vedotin as part of the SG035-0004 clinical study experienced an improvement in clinical benefit as measured by longer progression free survival (PFS) compared with their most recent prior line of therapy. Of the 17 patients (29%) who had B symptoms at baseline, 14 patients (82%) experienced resolution of all B symptoms in a median time from initiation of brentuximab vedotin of 0.7 months. The European Medicines Agency has deferred the obligation to submit the results of studies with Adcetris in one or more subsets of the paediatric population in the treatment of Hodgkin lymphoma and treatment of anaplastic large cell lymphoma (see section 4.2 for information on paediatric use). This medicinal product has been authorised under a so-called 'conditional approval' scheme. This means that further evidence on this medicinal product is awaited. The European Medicines Agency will review new information on this medicinal product at least every year and this SmPC will be updated as necessary. 5.2 Pharmacokinetic properties The pharmacokinetics of brentuximab vedotin were evaluated in phase 1 studies and in a population pharmacokinetic analysis of data from 314 patients. In all clinical trials, brentuximab vedotin was administered as an intravenous infusion. Maximum concentrations of brentuximab vedotin ADC were typically observed at the end of infusion or the sampling timepoint closest to the end of infusion. A multiexponential decline in ADC serum concentrations was observed with a terminal half-life of approximately 4 to 6 days. Exposures were approximately dose proportional. Minimal to no accumulation of ADC was observed with multiple doses at the every 3-week schedule, consistent with the terminal half-life estimate. Typical Cmax and AUC of ADC after a single 1.8 mg/kg in a phase 1 study was approximately 31.98 μg/ml and 79.41 μg/ml x day respectively. MMAE is the major metabolite of brentuximab vedotin. Median Cmax, AUC and Tmax of MMAE after a single 1.8 mg/kg of the ADC in a phase 1 study was approximately 4.97 ng/ml, 37.03 ng/ml x day and 2.09 days respectively. MMAE exposures decreased after multiple doses of brentuximab vedotin with approximately 50% to 80% of the exposure of the first dose being observed at subsequent doses. In the first cycle, higher MMAE exposure was associated with an absolute decrease in neutrophil count. Distribution In vitro, the binding of MMAE to human serum plasma proteins ranged from 68-82%. MMAE is not likely to displace or to be displaced by highly protein-bound medicines. In vitro, MMAE was a substrate of P-gp and was not an inhibitor of P-gp at clinical concentrations. In humans, the mean steady state volume of distribution was approximately 6-10 l for ADC. Based on population PK estimation the typical apparent volume of distribution (VM and VMP) of MMAE were 7.37 l and 36.4 l respectively. Metabolism The ADC is expected to be catabolised as a protein with component amino acids recycled or eliminated. In vivo data in animals and humans suggest that only a small fraction of MMAE released from brentuximab vedotin is metabolized. The levels of MMAE metabolites have not been measured in human plasma. At least one metabolite of MMAE has been shown to be active in vitro. MMAE is a substrate of CYP3A4 and possibly CYP2D6. In vitro data indicate that the MMAE metabolism that occurs is primarily via oxidation by CYP3A4/5. In vitro studies using human liver microsomes indicate that MMAE inhibits only CYP3A4/5 at concentrations much higher than was achieved during clinical application. MMAE does not inhibit other isoforms. MMAE did not induce any major CYP450 enzymes in primary cultures of human hepatocytes. Elimination The ADC is eliminated by catabolism with a typical estimated CL and half life of 1.457 l/day and 4-6 days respectively. The elimination of MMAE was limited by its rate of release from ADC, typical apparent CL and half life of MMAE was 19.99 l/day and 3-4 days respectively. An excretion study was undertaken in patients who received a dose of 1.8 mg/kg of brentuximab vedotin. Approximately 24% of the total MMAE administered as part of the ADC during a brentuximab vedotin infusion was recovered in both urine and faeces over a 1-week period. Of the recovered MMAE, approximately 72% was recovered in the faeces. A lesser amount of MMAE (28%) was excreted in the urine. Pharmacokinetics in special populations Population PK analysis showed that baseline serum albumin concentration was a significant covariate of MMAE clearance. The analysis indicated that MMAE clearance was 2-fold lower in patients with low serum albumin concentrations <3.0 g/dl compared with patients with serum albumin concentrations within the normal range. Hepatic impairment A study evaluated the PK of brentuximab vedotin and MMAE after the administration of 1.2 mg/kg of ADCETRIS to patients with mild (Child-Pugh A; n=1), moderate (Child-Pugh B; n=5) and severe (Child-Pugh C; n=1) hepatic impairment. Compared to patients with normal hepatic function, MMAE exposure increased approximately 2.3- fold (90% CI 1.27-4.12 fold) in patients with hepatic impairment. Renal impairment A study evaluated the PK of brentuximab vedotin and MMAE after the administration of 1.2 mg/kg of ADCETRIS to patients with mild (n=4), moderate (n=3) and severe (n=3) renal impairment. Compared to patients with normal renal function, MMAE exposure increased approximately 1.9-fold (90% CI 0.85-4.21 fold) in patients with severe renal impairment (creatinine clearance < 30 ml/min). No effect was observed in patients with mild or moderate renal impairment. Older patients Clinical studies of brentuximab vedotin did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. Paediatric population Clinical studies of brentuximab vedotin did not include sufficient numbers of patients below 18 years of age to determine whether the PK profile differs from adult patients. 5.3 Preclinical safety data MMAE has been shown to have aneugenic properties in an in vivo rat bone marrow micronucleus study. These results were consistent with the pharmacological effect of MMAE on the mitotic apparatus (disruption of the microtubule network) in cells. The effects of brentuximab vedotin on human male and female fertility have not been studied. However, results of repeat-dose toxicity studies in rats indicate the potential for brentuximab vedotin to impair male reproductive function and fertility. Testicular atrophy and degeneration were partially reversible following a 16-week treatment-free period. Brentuximab vedotin caused embryo-foetal lethality in pregnant female rats. In nonclinical studies, lymphoid depletion and reduced thymic weight were observed, consistent with the pharmacologic disruption of microtubules caused by MMAE derived from brentuximab vedotin. 6. Pharmaceutical particulars 6.1 List of excipients Citric acid monohydrate Sodium citrate dihydrate α,α-Trehalose dihydrate Polysorbate 80 6.2 Incompatibilities In the absence of compatibility studies, this medicinal product must not be mixed with other medicinal products except those mentioned in section 6.6. 6.3 Shelf life 3 years. After reconstitution/dilution, from a microbiological point of view, the product should be used immediately. However, chemical and physical in-use stability has been demonstrated for 24 hours at 2°C-8°C. 6.4 Special precautions for storage Store in a refrigerator (2°C-8°C). Do not freeze. Keep the vial in the original carton in order to protect from light. For storage conditions after reconstitution and dilution of the medicinal product, see section 6.3. 6.5 Nature and contents of container Type I glass vial with a butyl rubber stopper and an aluminium/plastic flip-off seal, containing 50 mg powder. Pack of 1 vial. 6.6 Special precautions for disposal and other handling General precautions Procedures for proper handling and disposal of anticancer medicines should be considered. Proper aseptic technique throughout the handling of this medicinal product should be followed. Instructions for reconstitution Each single use vial must be reconstituted with 10.5 ml of water for injections to a final concentration of 5 mg/ml. Each vial contains a 10% overfill giving 55 mg of ADCETRIS per vial and a total reconstituted volume of 11 mL. 1. Direct the stream toward the wall of the vial and not directly at the cake or powder. 2. Gently swirl the vial to aid dissolution. DO NOT SHAKE. 3. The reconstituted solution in the vial is a clear to slightly opalescent, colourless solution with a final pH of 6.6. 4. The reconstituted solution should be inspected visually for any foreign particulate matter and/or discoloration. In the event of either being observed, discard the medicinal product. Preparation of infusion solution The appropriate amount of reconstituted ADCETRIS must be withdrawn from the vial(s) and added to an infusion bag containing sodium chloride 9 mg/ml (0.9%) solution for injection in order to achieve a final concentration of 0.4-1.2 mg/ml ADCETRIS. The recommended diluent volume is 150 ml. The already reconstituted ADCETRIS can also be diluted into 5% dextrose for injection or Lactated Ringer's for injection. Gently invert the bag to mix the solution containing ADCETRIS. DO NOT SHAKE. Any portion left in the vial, after withdrawal of the volume to be diluted, must be disposed of in accordance with local requirements. Do not add other medicinal products to the prepared ADCETRIS infusion solution or intravenous infusion set. The infusion line should be flushed following administration with sodium chloride 9 mg/ml (0.9%) solution for injection, 5% dextrose for injection, or Lactated Ringer's for injection. Following dilution, infuse the ADCETRIS solution immediately at the recommended infusion rate. Total storage time of the solution from reconstitution to infusion should not exceed 24 hours. Determining dosage amount: Calculation to determine the total ADCETRIS dose (ml) to be further diluted (see section 4.2):
b. To be diluted in 150 ml of diluent and administered by intravenous infusion over 30 minutes every 3 weeks. c. If patient's weight is more than 100 kg, the dose calculation should use 100 kg. d. The maximal recommended dose is 180 mg. Disposal ADCETRIS is for single use only. Any unused product or waste material should be disposed of in accordance with local requirements. 7. Marketing authorisation holder Takeda Pharma A/S Langebjerg 1 DK-4000 Roskilde Denmark 8. Marketing authorisation number(s) EU/1/12/794/001 9. Date of first authorisation/renewal of the authorisation Date of first authorization: 25 October 2012 Date of renewal: 26 August 2013 10. Date of revision of the text 22 August 2014 Detailed information on this medicinal product is available on the website of the European Medicines Agency http://www.ema.europa.eu 美国食品和药品监督管理局2011年8月19日批准Adcetris(brentuximab vedotin)治疗霍杰金淋巴瘤(HL)和一种罕见淋巴瘤被称为系统性间变性大细胞淋巴瘤(ALCL). 淋巴瘤是淋巴系统癌症。Adcetris是一种抗体药物结合物,结合抗体和药物,允许抗体指引药物至淋巴瘤细胞上被称为D30靶点。 Adcetris被用于自身干细胞移植后或两次既往化疗后疾病有进展不能接受移植HL患者。自身干细胞移植是用患者自身骨髓的方法被设计修复高剂量化疗损伤骨髓。Adcetris还可用于1次既往化疗后疾病进展的ALCL患者。 FDA药物评价和研究中心肿瘤药品办公室主任Richard Pazdur, M.D.说“早期临床资料提示接受Adcetris患者对霍杰金淋巴瘤和全身间变性淋巴瘤治疗经受显著缓解”。 按照美国国立癌症研究所(NCI),霍杰金淋巴瘤(HL)的常见症状包括淋巴结,脾增大,发热,体重减轻,疲乏,或夜汗。NCI估计美国2011年新诊断8,830例和约1,300人将死于该病。按照NCI全身ALCL是一种罕见恶性肿瘤(非-霍奇金氏淋巴瘤)可见于机体几个部位包括淋巴结,皮肤,骨,软组织,肺或肝。 Adcetris是自1977年第一个被FDA-批准治疗霍杰金淋巴瘤和第一个专门适用于治疗ALCL的新药。 在一项单个临床试验涉及102例患者中评价HL患者中Adcetris的有效性。在单组试验中,患者只被Adcetris治疗。研究主要终点是客观缓解率,治疗后经受完全或部分癌症皱缩或消失患者的百分率。对治疗73%患者达到或完全或部分缓解。这些患者对治疗缓解平均6.7个月。 在一项单次临床试验中在58例患者中评价Adcetris在全身ALCL患者中的有效性。在单组试验中,患者只用Adcetris治疗。与霍奇金氏淋巴瘤试验相似,试验主要终点是客观缓解率。为ALCL接受Adcetris患者中,86%经受或完全或部分缓解和平均缓解12.6个月。 经受Adcetris最常见副作用是对抗感染白细胞减低(中性粒细胞减少),神经损伤(周边感觉神经病变),疲乏,恶心,贫血,上呼吸道感染,腹泻,发热,咳嗽,呕吐,和血小板低水平 (血小板减少)。 ------------------------------------------------------- 注:以下产品不同国家上市,价格不同,购买以咨询为准 ------------------------------------------------------- 产地国家:美国 原产地英文商品名: ADCETRIS 50MG/VIAL 原产地英文药品名: BRENTUXIMAB VEDOTIN 中文参考商品译名: ADCETRIS 50毫克/瓶 中文参考药品译名: brentuximab vedotin 生产厂家中文参考译名: 西雅图遗传技术公司 生产厂家英文名: SEATTLE GENETICS
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||