|
当前位置:新特药品资料下载首页 >> 新特药品PDF说明书 >> 注射用顺铂冻干粉针剂cisplatin(Platinol)
注射用顺铂冻干粉针剂cisplatin(Platinol)
cisplatin (Platinol) 【用法】静脉注射,1次20mg,溶于生理盐水30ml中,1日1次或隔日1次,一疗程总量100mg。或溶于氯化钠注射液500ml中滴注,连用5天,或每次30mg/m2,每日1次,连用3天,间隔3~4周可再重复给药。或以高剂量80~120mg/m2静脉滴注,每3~4周重复1次,需配合水化利尿,使尿量保持在2000~3000ml。本品亦可动脉注射或胸、腹腔内注射。 【注意】不良反应主要为消化道反应、肾脏毒性、骨髓抑制及听神经毒性,与所用剂量的大小及总量有关。少数病人并有胰腺毒性可诱发糖尿。因此,在用本品前,尤其是高剂量时,应先检查肾脏功能及听力,并注意多饮水或输液强迫利尿。肾功能不全者慎用。 Package Insert
DESCRIPTIONCisplatin Injection is a clear, light-yellow, sterile aqueous solution available in amber vials containing 1 mg/mL of cisplatin. One mL of infusion concentrate 1 mg/mL contains: 1 mg cisplatin, 9 mg sodium chloride, hydrochloric acid and/or sodium hydroxide to pH of 3.2-4.4, and water for injection. The active ingredient, cisplatin, is a yellow to orange crystalline powder with the molecular formula PtCl2H6N2 and a molecular weight of 300.1. Cisplatin is a heavy metal complex containing a central atom of platinum surrounded by two chloride atoms and two ammonia molecules in the cis position. It is soluble in water or saline at 1 mg/mL and in dimethylformamide at 24 mg/mL. It has a melting point of 207°C. CLINICAL PHARMACOLOGYPlasma concentrations of the parent compound, cisplatin, decay monoexponentially with a half-life of about 20 to 30 minutes following bolus administrations of 50 or 100 mg/m2 doses. Monoexponential decay and plasma half-lives of about 0.5 hour are also seen following 2-hour or 7-hour infusions of 100 mg/m2. After the latter, the total-body clearances and volumes of distribution at steady-state for cisplatin are about 15 to 16 L/h/m2 and 11 to 12 L/m2. Due to its unique chemical structure, the chlorine atoms of cisplatin are more subject to chemical displacement reactions by nucleophiles, such as water or sulfhydryl groups, than to enzyme-catalyzed metabolism. At physiological pH in the presence of 0.1M NaCl, the predominant molecular species are cisplatin and monohydroxymonochloro cis-diammine platinum (ll) in nearly equal concentrations. The latter, combined with the possible direct displacement of the chlorine atoms by sulfhydryl groups of amino acids or proteins, accounts for the instability of cisplatin in biological matrices. The ratios of cisplatin to total free (ultrafilterable) platinum in the plasma vary considerably between patients and range from 0.5 to 1.1 after a dose of 100 mg/m2. Cisplatin does not undergo the instantaneous and reversible binding to plasma proteins that is characteristic of normal drug-protein binding. However, the platinum from cisplatin, but not cisplatin itself, becomes bound to several plasma proteins, including albumin, transferrin, and gamma globulin. Three hours after a bolus injection and two hours after the end of a three-hour infusion, 90% of the plasma platinum is protein bound. The complexes between albumin and the platinum from cisplatin do not dissociate to a significant extent and are slowly eliminated with a minimum half-life of five days or more. Following cisplatin doses of 20 to 120 mg/m2, the concentrations of platinum are highest in liver, prostate, and kidney; somewhat lower in bladder, muscle, testicle, pancreas, and spleen; and lowest in bowel, adrenal, heart, lung, cerebrum, and cerebellum. Platinum is present in tissues for as long as 180 days after the last administration. With the exception of intracerebral tumors, platinum concentrations in tumors are generally somewhat lower than the concentrations in the organ where the tumor is located. Different metastatic sites in the same patient may have different platinum concentrations. Hepatic metastases have the highest platinum concentrations, but these are similar to the platinum concentrations in normal liver. Maximum red blood cell concentrations of platinum are reached within 90 to 150 minutes after a 100 mg/m2 dose of cisplatin and decline in a biphasic manner with a terminal half-life of 36 to 47 days. Over a dose range of 40 to 140 mg cisplatin/m2 given as a bolus injection or as infusions varying in length from 1 hour to 24 hours, from 10% to about 40% of the administered platinum is excreted in the urine in 24 hours. Over five days following administration of 40 to 100 mg/m2 doses given as rapid, 2 to 3 hour, or 6 to 8 hour infusions, a mean of 35% to 51% of the dosed platinum is excreted in the urine. Similar mean urinary recoveries of platinum of about 14% to 30% of the dose are found following five daily administrations of 20, 30, or 40 mg/m2/day. Only a small percentage of the administered platinum is excreted beyond 24 hours post-infusion and most of the platinum excreted in the urine in 24 hours is excreted within the first few hours. Platinum-containing species excreted in the urine are the same as those found following the incubation of cisplatin with urine from healthy subjects, except that the proportions are different. The parent compound, cisplatin, is excreted in the urine and accounts for 13% to 17% of the dose excreted within one hour after administration of 50 mg/m2. The mean renal clearance of cisplatin exceeds creatinine clearance and is 62 and 50 mL/min/m2 following administration of 100 mg/m2 as 2 hour or 6 to 7 hour infusions, respectively. The renal clearance of free (ultrafilterable) platinum also exceeds the glomerular filtration rate indicating that cisplatin or other platinum-containing molecules are actively secreted by the kidneys. The renal clearance of free platinum is nonlinear and variable and is dependent on dose, urine flow rate, and individual variability in the extent of active secretion and possible tubular reabsorption. There is a potential for accumulation of ultrafilterable platinum plasma concentrations whenever cisplatin is administered on a daily basis but not when dosed on an intermittent basis. No significant relationships exist between the renal clearance of either free platinum or cisplatin and creatinine clearance. Although small amounts of platinum are present in the bile and large intestine after administration of cisplatin, the fecal excretion of platinum appears to be insignificant. INDICATIONSCisplatin Injection is indicated as therapy to be employed as follows: Metastatic Testicular TumorsIn established combination therapy with other approved chemotherapeutic agents in patients with metastatic testicular tumors who have already received appropriate surgical and/or radiotherapeutic procedures. Metastatic Ovarian TumorsIn established combination therapy with other approved chemotherapeutic agents in patients with metastatic ovarian tumors who have already received appropriate surgical and/or radiotherapeutic procedures. An established combination consists of Cisplatin Injection and cyclophosphamide injection. Cisplatin Injection, as a single agent, is indicated as secondary therapy in patients with metastatic ovarian tumors refractory to standard chemotherapy who have not previously received Cisplatin Injection therapy. Advanced Bladder CancerCisplatin Injection is indicated as a single agent for patients with transitional cell bladder cancer which is no longer amenable to local treatments, such as surgery and/or radiotherapy. CONTRAINDICATIONSCisplatin is contraindicated in patients with preexisting renal impairment. Cisplatin should not be employed in myelosuppressed patients, or patients with hearing impairment. Cisplatin is contraindicated in patients with a history of allergic reactions to cisplatin or other platinum-containing compounds. WARNINGSCisplatin produces cumulative nephrotoxicity which is potentiated by aminoglycoside antibiotics. The serum creatinine, BUN, creatinine clearance, and magnesium, sodium, potassium, and calcium levels should be measured prior to initiating therapy, and prior to each subsequent course. At the recommended dosage, cisplatin should not be given more frequently than once every 3 to 4 weeks (see ADVERSE REACTIONS). Elderly patients may be more susceptible to nephrotoxicity (see PRECAUTIONS: Geriatric Use). There are reports of severe neuropathies in patients in whom regimens are employed using higher doses of cisplatin or greater dose frequencies than those recommended. These neuropathies may be irreversible and are seen as paresthesias in a stocking-glove distribution, areflexia, and loss of proprioception and vibratory sensation. Elderly patients may be more susceptible to peripheral neuropathy (see PRECAUTIONS: Geriatric Use). Loss of motor function has also been reported. Anaphylactic-like reactions to cisplatin have been reported. These reactions have occurred within minutes of administration to patients with prior exposure to cisplatin, and have been alleviated by administration of epinephrine, corticosteroids, and antihistamines. Since ototoxicity of cisplatin is cumulative, audiometric testing should be performed prior to initiating therapy and prior to each subsequent dose of drug (see ADVERSE REACTIONS). Cisplatin can cause fetal harm when administered to a pregnant woman. Cisplatin is mutagenic in bacteria and produces chromosome aberrations in animal cells in tissue culture. In mice cisplatin is teratogenic and embryotoxic. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Patients should be advised to avoid becoming pregnant. The carcinogenic effect of cisplatin was studied in BD IX rats. Cisplatin was administered i.p. to 50 BD IX rats for 3 weeks, 3 × 1 mg/kg body weight per week. Four hundred and fifty-five days after the first application, 33 animals died, 13 of them related to malignancies: 12 leukemias and 1 renal fibrosarcoma. The development of acute leukemia coincident with the use of cisplatin has been reported rarely in humans. In these reports, cisplatin was generally given in combination with other leukemogenic agents. PRECAUTIONSPeripheral blood counts should be monitored weekly. Liver function should be monitored periodically. Neurologic examination should also be performed regularly (see ADVERSE REACTIONS). Drug InteractionsPlasma levels of anticonvulsant agents may become subtherapeutic during cisplatin therapy. In a randomized trial in advanced ovarian cancer, response duration was adversely affected when pyridoxine was used in combination with altretamine (hexamethylmelamine) and cisplatin. Carcinogenesis, Mutagenesis, Impairment of FertilitySee WARNINGS. PregnancyPregnancy Category DSee WARNINGS. Nursing MothersCisplatin has been reported to be found in human milk; patients receiving cisplatin should not breast feed. Pediatric UseSafety and effectiveness in pediatric patients have not been established. Geriatric UseInsufficient data are available from clinical trials of cisplatin in the treatment of metastatic testicular tumors or advanced bladder cancer to determine whether elderly patients respond differently than younger patients. In four clinical trials of combination chemotherapy for advanced ovarian carcinoma, 1484 patients received cisplatin either in combination with cyclophosphamide or paclitaxel. Of these, 426 (29%) were older than 65 years. In these trials, age was not found to be a prognostic factor for survival. However, in a later secondary analysis for one of these trials, elderly patients were found to have shorter survival compared with younger patients. In all four trials, elderly patients experienced more severe neutropenia than younger patients. Higher incidences of severe thrombocytopenia and leukopenia were also seen in elderly compared with younger patients, although not in all cisplatin-containing treatment arms. In the two trials where nonhematologic toxicity was evaluated according to age, elderly patients had a numerically higher incidence of peripheral neuropathy than younger patients. Other reported clinical experience suggests that elderly patients may be more susceptible to myelosuppression, infectious complications, and nephrotoxicity than younger patients. Cisplatin is known to be substantially excreted by the kidney and is contraindicated in patients with preexisting renal impairment. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and renal function should be monitored. ADVERSE REACTIONSNephrotoxicityDose-related and cumulative renal insufficiency, including acute renal failure, is the major dose-limiting toxicity of cisplatin. Renal toxicity has been noted in 28% to 36% of patients treated with a single dose of 50 mg/m2. It is first noted during the second week after a dose and is manifested by elevations in BUN and creatinine, serum uric acid and/or a decrease in creatinine clearance. Renal toxicity becomes more prolonged and severe with repeated courses of the drug. Renal function must return to normal before another dose of cisplatin can be given. Elderly patients may be more susceptible to nephrotoxicity (see PRECAUTIONS: Geriatric Use). Impairment of renal function has been associated with renal tubular damage. The administration of cisplatin using a 6- to 8-hour infusion with intravenous hydration, and mannitol has been used to reduce nephrotoxicity. However, renal toxicity still can occur after utilization of these procedures. OtotoxicityOtotoxicity has been observed in up to 31% of patients treated with a single dose of cisplatin 50 mg/m2, and is manifested by tinnitus and/or hearing loss in the high frequency range (4000 to 8000 Hz). Decreased ability to hear normal conversational tones may occur occasionally. Deafness after the initial dose of cisplatin has been reported rarely. Ototoxic effects may be more severe in children receiving cisplatin. Hearing loss can be unilateral or bilateral and tends to become more frequent and severe with repeated doses. Ototoxicity may be enhanced with prior or simultaneous cranial irradiation. It is unclear whether cisplatin induced ototoxicity is reversible. Ototoxic effects may be related to the peak plasma concentration of cisplatin. Careful monitoring of audiometry should be performed prior to initiation of therapy and prior to subsequent doses of cisplatin. Vestibular toxicity has also been reported. Ototoxicity may become more severe in patients being treated with other drugs with nephrotoxic potential. HematologicMyelosuppression occurs in 25% to 30% of patients treated with cisplatin. The nadirs in circulating platelets and leukocytes occur between days 18 to 23 (range 7.5 to 45) with most patients recovering by day 39 (range 13 to 62). Leukopenia and thrombocytopenia are more pronounced at higher doses (>50 mg/m2). Anemia (decrease of 2 g hemoglobin/100 mL) occurs at approximately the same frequency and with the same timing as leukopenia and thrombocytopenia. Fever and infection have also been reported in patients with neutropenia. Potential fatalities due to infection (secondary to myelosuppression) have been reported as part of postmarketing surveillance. Elderly patients may be more susceptible to myelosuppression (see PRECAUTIONS: Geriatric Use). In addition to anemia secondary to myelosuppression, a Coombs' positive hemolytic anemia has been reported. In the presence of cisplatin hemolytic anemia, a further course of treatment may be accompanied by increased hemolysis and this risk should be weighed by the treating physician. The development of acute leukemia coincident with the use of cisplatin has been reported rarely in humans. In these reports, cisplatin was generally given in combination with other leukemogenic agents. GastrointestinalMarked nausea and vomiting occur in almost all patients treated with cisplatin, and are occasionally so severe that the drug must be discontinued. Nausea and vomiting usually begin within 1 to 4 hours after treatment and last up to 24 hours. Various degrees of vomiting, nausea and/or anorexia may persist for up to 1 week after treatment. Delayed nausea and vomiting (begins or persists 24 hours or more after chemotherapy) has occurred in patients attaining complete emetic control on the day of cisplatin therapy. Diarrhea has also been reported. OTHER TOXICITIESVascular toxicities coincident with the use of cisplatin in combination with other antineoplastic agents have been reported rarely. The events are clinically heterogeneous and may include myocardial infarction, cerebrovascular accident, thrombotic microangiopathy (HUS), or cerebral arteritis. Various mechanisms have been proposed for these vascular complications. There are also reports of Raynaud's phenomenon occurring in patients treated with the combination of bleomycin, vinblastine with or without cisplatin. It has been suggested that hypomagnesemia developing coincident with the use of cisplatin may be an added, although not essential, factor associated with this event. However, it is currently unknown if the cause of Raynaud's phenomenon in these cases is the disease, underlying vascular compromise, bleomycin, vinblastine, hypomagnesemia, or a combination of any of these factors. Serum Electrolyte DisturbancesHypomagnesemia, hypocalcemia, hyponatremia, hypokalemia, and hypophosphatemia have been reported to occur in patients treated with cisplatin and are probably related to renal tubular damage. Tetany has been reported occasionally in those patients with hypocalcemia and hypomagnesemia. Generally, normal serum electrolyte levels are restored by administering supplemental electrolytes and discontinuing cisplatin. Inappropriate antidiuretic hormone syndrome has also been reported. HyperuricemiaHyperuricemia has been reported to occur at approximately the same frequency as the increases in BUN and serum creatinine. It is more pronounced after doses greater than 50 mg/m2, and peak levels of uric acid generally occur between 3 to 5 days after the dose. Allopurinol therapy for hyperuricemia effectively reduces uric acid levels. NeurotoxicitySee WARNINGS. Neurotoxicity, usually characterized by peripheral neuropathies, has been reported. The neuropathies usually occur after prolonged therapy (4 to 7 months); however, neurologic symptoms have been reported to occur after a single dose. Although symptoms and signs of cisplatin neuropathy usually develop during treatment, symptoms of neuropathy may begin 3 to 8 weeks after the last dose of cisplatin, although this is rare. Cisplatin therapy should be discontinued when the symptoms are first observed. The neuropathy, however, may progress further even after stopping treatment. Preliminary evidence suggests peripheral neuropathy may be irreversible in some patients. Elderly patients may be more susceptible to peripheral neuropathy (see PRECAUTIONS: Geriatric Use). Lhermitte's sign, dorsal column myelopathy, and autonomic neuropathy have also been reported. Loss of taste and seizures have also been reported. Muscle cramps, defined as localized, painful, involuntary skeletal muscle contractions of sudden onset and short duration, have been reported and were usually associated in patients receiving a relatively high cumulative dose of cisplatin and with a relatively advanced symptomatic stage of peripheral neuropathy. Ocular ToxicityOptic neuritis, papilledema, and cerebral blindness have been reported infrequently in patients receiving standard recommended doses of cisplatin. Improvement and/or total recovery usually occurs after discontinuing cisplatin. Steroids with or without mannitol have been used; however, efficacy has not been established. Blurred vision and altered color perception have been reported after the use of regimens with higher doses of cisplatin or greater dose frequencies than recommended in the package insert. The altered color perception manifests as a loss of color discrimination, particularly in the blue-yellow axis. The only finding on funduscopic exam is irregular retinal pigmentation of the macular area. Anaphylactic-Like ReactionsAnaphylactic-like reactions have been reported occasionally in patients previously exposed to cisplatin. The reactions consist of facial edema, wheezing, tachycardia, and hypotension within a few minutes of drug administration. Reactions may be controlled by intravenous epinephrine with corticosteroids and/or antihistamines as indicated. Patients receiving cisplatin should be observed carefully for possible anaphylactic-like reactions and supportive equipment and medication should be available to treat such a complication. HepatotoxicityTransient elevations of liver enzymes, especially SGOT, as well as bilirubin, have been reported to be associated with cisplatin administration at the recommended doses. Other EventsOther toxicities reported to occur infrequently are cardiac abnormalities, hiccups, elevated serum amylase, and rash. Alopecia, malaise, asthenia, and dehydration have been reported as part of postmarketing surveillance. Local soft tissue toxicity has been reported rarely following extravasation of cisplatin. Severity of the local tissue toxicity appears to be related to the concentration of the cisplatin solution. Infusion of solutions with a cisplatin concentration greater than 0.5 mg/mL may result in tissue cellulitis, fibrosis, and necrosis. OVERDOSAGECaution should be exercised to prevent inadvertent overdosage with cisplatin. Acute overdosage with this drug may result in kidney failure, liver failure, deafness, ocular toxicity (including detachment of the retina), significant myelosuppression, intractable nausea and vomiting and/or neuritis. In addition, death can occur following overdosage. No proven antidotes have been established for cisplatin overdosage. Hemodialysis, even when initiated four hours after the overdosage, appears to have little effect on removing platinum from the body because of cisplatin's rapid and high degree of protein binding. Management of overdosage should include general supportive measures to sustain the patient through any period of toxicity that may occur. DOSAGE AND ADMINISTRATIONNote: Needles or intravenous sets containing aluminum parts that may come in contact with cisplatin should not be used for preparation or administration. Aluminum reacts with cisplatin, causing precipitate formation and a loss of potency. Metastatic Testicular TumorsThe usual cisplatin dose for the treatment of testicular cancer in combination with other approved chemotherapeutic agents is 20 mg/m2 IV daily for 5 days per cycle. Metastatic Ovarian TumorsThe usual cisplatin dose for the treatment of metastatic ovarian tumors in combination with cyclophosphamide injection is 75–100 mg/m2 IV per cycle once every four weeks (DAY 1). The dose of cyclophosphamide injection when used in combination with cisplatin is 600 mg/m2 IV once every 4 weeks (DAY 1). For directions for the administration of cyclophosphamide injection, refer to the cyclophosphamide package insert. In combination therapy, cisplatin and cyclophosphamide injection are administered sequentially. As a single agent, cisplatin should be administered at a dose of 100 mg/m2 IV per cycle once every four weeks. Advanced Bladder CancerCisplatin should be administered as a single agent at a dose of 50 to 70 mg/m2 IV per cycle once every 3 to 4 weeks depending on the extent of prior exposure to radiation therapy and/or prior chemotherapy. For heavily pretreated patients an initial dose of 50 mg/m2 per cycle repeated every 4 weeks is recommended. All PatientsPretreatment hydration with 1 to 2 liters of fluid infused for 8 to 12 hours prior to a cisplatin dose is recommended. The drug is then diluted in 2 liters of 5% Dextrose in ½ to ⅓ normal saline containing 37.5 g of mannitol, and infused over a 6- to 8-hour period. If diluted solution is not to be used within 6 hours, protect solution from light. Do not dilute cisplatin in just 5% Dextrose Injection. Adequate hydration and urinary output must be maintained during the following 24 hours. A repeat course of cisplatin should not be given until the serum creatinine is below 1.5 mg/100 mL, and/or the BUN is below 25 mg/100 mL. A repeat course should not be given until circulating blood elements are at an acceptable level (platelets ≥ 100,000/mm3, WBC ≥ 4,000/mm3). Subsequent doses of cisplatin should not be given until an audiometric analysis indicates that auditory acuity is within normal limits. As with other potentially toxic compounds, caution should be exercised in handling the aqueous solution. Skin reactions associated with accidental exposure to cisplatin may occur. The use of gloves is recommended. If cisplatin contacts the skin or mucosa, immediately and thoroughly wash the skin with soap and water and flush the mucosa with water. The aqueous solution should be used intravenously only and should be administered by IV infusion over a 6- to 8-hour period. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. NOTE TO PHARMACISTExercise caution to prevent inadvertent cisplatin overdosage. Please call prescriber if dose is greater than 100 mg/m2 per cycle. Aluminum and flip-off seal of vial have been imprinted with the following statement: CALL DR. IF DOSE >100 MG/M2/CYCLE. STABILITYCisplatin Injection is a sterile, multiple dose vial without preservatives. Store at 15°–25°C (59°–77°F). Do not refrigerate. Protect unopened container from light. The cisplatin remaining in the amber vial following initial entry is stable for 28 days protected from light or for 7 days under fluorescent room light. Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1-8 There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate. To minimize the risk of dermal exposure, always wear impervious gloves when handling vials containing Cisplatin Injection. This includes all handling activities in clinical settings, pharmacies, storerooms, and home healthcare settings, including during unpacking and inspection, transport within a facility, and dose preparation and administration. HOW SUPPLIEDCisplatin Injection, 1 mg/mL, is supplied in multiple dose vials containing 50 mL and 100 mL.
REFERENCES
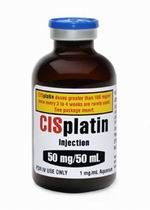
Issued: July 2008 Manufactured for: Manufactured by: 93.134.420-B PRINCIPAL DISPLAY PANEL - 50 mg/50 mL Vial LabelCISplatin doses greater than 100 mg/m2 once every NDC 0703-5747-11 CISplatin 50 mg/50 mL 50 mL Multiple Dose Vial TEVA |
最新下载推荐下载
下载排行 |

|
 |
|
| 新特药品资料下载首页 | 药品季度价格表下载 | 新特药品PDF说明书 | 分类 | 专题 | 留言本 | 投稿 | 搜索 |