|
2014年2月24日,美国食品药品监督管理局(FDA)批准Myalept(重组甲硫氨酰-人类瘦蛋白metreleptin)注射用作为替代治疗为治疗瘦蛋白缺乏的并发症,除了饮食,在有先天性全身性或获得性全身性脂肪代谢障碍患者。
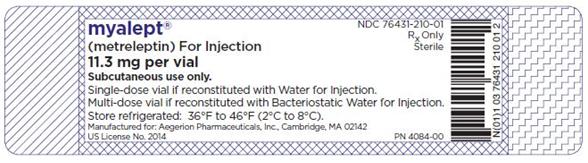
Instruct patients that if a dose is missed, administer the dose as soon as noticed, and resume the normal dosing schedule the next day. 2.2 MYALEPT Preparation and Storage Healthcare practitioners should provide proper training to patients and caregivers regarding how to prepare and administer the correct dose of MYALEPT prior to self-use. The patients and caregivers should prepare and administer the first dose of MYALEPT under the supervision of a qualified healthcare professional. Instruct patients to store the vials of lyophilized powder in their carton in the refrigerator as soon as received [see How Supplied/Storage and Handling (16.2)]. MYALEPT can be reconstituted aseptically with 2.2 mL of sterile Bacteriostatic Water for Injection (BWFI), USP (0.9% benzyl alcohol), or with 2.2 mL of sterile Water for Injection (WFI). When reconstituted in BWFI, MYALEPT solution can be used within 3 days when stored in the refrigerator between 36°F and 46°F (2°C and 8°C) and protected from light [see How Supplied/Storage and Handling (16.2)]. Discard unused reconstituted solution after 3 days. Attach the supplied sticker to the vial and enter the discard date. For use in neonates and infants, reconstitute with preservative-free sterile WFI [see Warnings and Precautions (5.7) and Use in Specific Populations (8.4)]. When reconstituted in sterile WFI, MYALEPT should be administered immediately. Unused reconstituted solution cannot be saved for later use and should be discarded. Reconstitution of the Lyophilized Powder Instruct patients to follow the directions below for reconstitution of the lyophilized powder: a) Remove the vial containing the MYALEPT lyophilized powder from the refrigerator and allow the vial to warm to room temperature prior to use. b) Visually inspect the vial containing MYALEPT. The cake of lyophilized powder should be intact and white in color. c) Using a 3-mL syringe with a 22-gauge or smaller diameter needle withdraw 2.2 mL of sterile Bacteriostatic Water for Injection (BWFI) or preservative-free sterile Water for Injection (WFI). Do not reconstitute MYALEPT with other diluents. d) Inject the BWFI or WFI into the vial containing the lyophilized powder of MYALEPT, slowly injecting down the side of the vial. It is normal for some bubbles to form. e) Remove the needle and syringe from the vial and gently swirl the contents to reconstitute. Do not shake or vigorously agitate. When properly mixed, the MYALEPT reconstituted solution should be clear and free of clumps or dry powder, bubbles or foam. Do not use the solution if discolored or cloudy, or if particulate matter remains. f) Regarding the compatibility of MYALEPT reconstituted solution with other solutions: • Do not mix with, or transfer into, the contents of another vial of MYALEPT. • Do not add other medications, including insulin. Use a separate syringe for insulin injections. See the MYALEPT Instructions for Use for complete administration instructions. The instructions can also be found at www.myalept.com. 2.3 Administration Instructions Healthcare practitioners should instruct patients and caregivers on the proper subcutaneous injection technique with care to avoid intramuscular injection in patients with minimal subcutaneous adipose tissue. Never administer MYALEPT intravenously or intramuscularly. Instruct patients to follow the recommended injection technique: a) Using a 1-mL syringe with a needle appropriate for subcutaneous injection, withdraw the prescribed dose of MYALEPT reconstituted solution. b) Remove any large air pockets or large bubbles from the filled syringe prior to administration. Some small bubbles may remain in the syringe. c) Administer MYALEPT into the subcutaneous tissue of the abdomen, thigh or upper arm. Advise patients to use a different injection site each day when injecting in the same region. After choosing an injection site, pinch the skin and at a 45-degree angle, inject the MYALEPT reconstituted solution subcutaneously. Avoid intramuscular injection, especially in patients with minimal subcutaneous adipose tissue. d) Doses exceeding 1 mL can be administered as two injections (the total daily dose divided equally) to minimize potential injection-site discomfort due to injection volume. When dividing doses due to volume, doses can be administered one after the other. Do not mix MYALEPT with insulin. Use a separate syringe for each medication. If MYALEPT and insulin are administered at the same time of day, they may be injected in the same body area using two different injection sites. See the MYALEPT Instructions for Use for complete administration instructions. The instructions can also be found at www.myalept.com. 2.4 Dosage Adjustments of Medications Known to Cause Hypoglycemia Dosage adjustments, including possible large reductions, of insulin or insulin secretagogue (e.g., sulfonylurea) may be necessary in some patients to minimize the risk of hypoglycemia [see Warnings and Precautions (5.4) and Adverse Reactions (6.1)]. Closely monitor blood glucose in patients on concomitant insulin therapy, especially those on high doses, or insulin secretagogue (e.g., sulfonylurea) when treating with MYALEPT. 2.5 Discontinuation in Patients at Risk for Pancreatitis When discontinuing MYALEPT therapy in patients with risk factors for pancreatitis (e.g., history of pancreatitis, severe hypertriglyceridemia), tapering of the dose over a one-week period is recommended. During tapering, monitor triglyceride levels and consider initiating or adjusting the dose of lipid-lowering medications as needed. Signs and/or symptoms consistent with pancreatitis should prompt an appropriate clinical evaluation. 3 DOSAGE FORMS AND STRENGTHS For Injection: 11.3 mg of metreleptin supplied in a vial as a sterile, white, solid, lyophilized cake (delivers 5 mg per mL of metreleptin when reconstituted with 2.2 mL of BWFI or WFI). 4 CONTRAINDICATIONS 4.1 General Obesity MYALEPT is contraindicated in patients with general obesity not associated with congenital leptin deficiency. MYALEPT has not been shown to be effective in treating general obesity, and the development of anti-metreleptin antibodies with neutralizing activity has been reported in obese patients treated with MYALEPT [see Warnings and Precautions (5.1)]. 4.2 Hypersensitivity MYALEPT is contraindicated in patients with prior severe hypersensitivity reactions to metreleptin or to any of the product components. Known hypersensitivity reactions have included urticaria and generalized rash [see Warnings and Precautions (5.6)]. 5 WARNINGS AND PRECAUTIONS 5.1 Risk for Development of Antibodies that Neutralize Endogenous Leptin and/or MYALEPT Anti-metreleptin antibodies with in vitro neutralizing activity to leptin associated with adverse events consistent with loss of endogenous leptin activity and/or loss of efficacy have been identified in two patients with generalized lipodystrophy treated with MYALEPT (severe infections, increases in HbA1c and triglycerides), and in three patients without lipodystrophy who received MYALEPT in clinical studies (excessive weight gain, development of glucose intolerance or diabetes mellitus). The clinical implications associated with development of anti-metreleptin antibodies with neutralizing activity are not well characterized at this time due to the small number of reports. Test for anti-metreleptin antibodies with neutralizing activity in patients who develop severe infections or show signs suspicious for loss of MYALEPT efficacy during treatment. Contact AstraZeneca at 1-866-216-1526 for neutralizing antibody testing of clinical samples [see Adverse Reactions (6.2)]. 5.2 Lymphoma Three cases of T-cell lymphoma have been reported in the MYALEPT lipodystrophy program; all three patients had acquired generalized lipodystrophy. Two of these patients were diagnosed with peripheral T-cell lymphoma while receiving MYALEPT. Both had immunodeficiency and significant hematologic abnormalities including severe bone marrow abnormalities before the start of MYALEPT treatment. A separate case of anaplastic large cell lymphoma was reported in a patient receiving MYALEPT who did not have hematological abnormalities before treatment. Lymphoproliferative disorders, including lymphomas, have been reported in patients with acquired generalized lipodystrophy not treated with MYALEPT. A causal relationship between MYALEPT treatment and the development and/or progression of lymphoma has not been established. Acquired lipodystrophies are associated with autoimmune disorders, and autoimmune disorders are associated with an increased risk of malignancies including lymphomas. The benefits and risks of MYALEPT treatment should be carefully considered in patients with acquired generalized lipodystrophy and/or those with significant hematologic abnormalities (including leukopenia, neutropenia, bone marrow abnormalities, lymphoma, and/or lymphadenopathy). 5.3 MYALEPT REMS Program MYALEPT is available only through a restricted distribution program under a REMS, called the MYALEPT REMS Program, because of the risks associated with the development of anti-metreleptin antibodies that neutralize endogenous leptin and/or MYALEPT and the risk for lymphoma [see Warnings and Precautions (5.1, 5.2)]. Notable requirements of the MYALEPT REMS Program include the following: • Prescribers must be certified with the program by enrolling and completing training. • Pharmacies must be certified with the program and only dispense MYALEPT after receipt of the MYALEPT REMS Prescription Authorization Form for each new prescription. Further information is available at www.myaleptrems.com or 1-855-6MYALEPT. 5.4 Hypoglycemia with Concomitant Use with Insulin and Insulin Secretagogues Dosage adjustments, including possible large reductions, of insulin or insulin secretagogue (e.g., sulfonylurea) may be necessary in some patients to minimize the risk of hypoglycemia [see Dosage and Administration (2.4) and Adverse Reactions (6.1)]. Closely monitor blood glucose in patients on concomitant insulin therapy, especially those on high doses, or insulin secretagogue (e.g., sulfonylurea), when treating with MYALEPT. 5.5 Autoimmunity Leptin plays a role in immune system homeostasis. Acquired lipodystrophies are associated with autoimmune disorders including autoimmune hepatitis and membranoproliferative glomerulonephritis. Cases of progression of autoimmune hepatitis and membranoproliferative glomerulonephritis (associated with massive proteinuria and renal failure) were observed in some patients with acquired generalized lipodystrophy treated with MYALEPT. A causal relationship between MYALEPT treatment and the development and/or progression of autoimmune disease has not been established. The potential benefits and risks of MYALEPT treatment should be carefully considered in patients with autoimmune disease. 5.6 Hypersensitivity There have been reports of generalized hypersensitivity (e.g., urticaria or generalized rash) in patients taking MYALEPT. If a hypersensitivity reaction occurs, instruct the patient to promptly seek medical advice regarding discontinuation of MYALEPT. 5.7 Benzyl Alcohol Toxicity MYALEPT contains benzyl alcohol when reconstituted with BWFI. MYALEPT contains no preservative when reconstituted with sterile Water for Injection (WFI). Preservative-free WFI is recommended for use in neonates and infants. The preservative benzyl alcohol has been associated with serious adverse events and death in pediatric patients, particularly in neonates and premature infants [see Use in Specific Populations (8.4)]. 6 ADVERSE REACTIONS 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. Open-Label, Single-Arm Study The safety of MYALEPT was evaluated in 48 patients with generalized lipodystrophy in a single-arm, open-label study [see Clinical Studies (14.1)]. The median duration of exposure in this trial was 2.7 years with a range of 3.6 months to 10.9 years. The most frequent adverse reactions are summarized in Table 2. Table 2: Adverse Reactions of 5% or Greater Incidence in Patients with Generalized Lipodystrophy Receiving MYALEPT in an Open-Label, Single-Arm Study
In patients with generalized lipodystrophy receiving MYALEPT in this study, less common adverse reactions included injection-site erythema and urticaria (N=2 [4%]). Six patients (13%) had 7 adverse reactions of hypoglycemia, 6 of which occurred in the setting of concomitant insulin use, with or without oral antihyperglycemic agents. Two patients (4%) had events of pancreatitis, both of whom had a medical history of pancreatitis. 6.2 Immunogenicity As with all therapeutic proteins, there is potential for immunogenicity. Anti-metreleptin antibodies were detected in 84% (36/43) of generalized lipodystrophy patients studied in the MYALEPT trials. Total anti-metreleptin antibody titers ranged between 1:5 and 1:1,953,125. The incompleteness of the current immunogenicity database precludes understanding of the magnitude and persistence of the observed anti-drug antibody responses. Anti-metreleptin antibodies with neutralizing activity associated with adverse events consistent with loss of endogenous leptin activity and/or loss of MYALEPT efficacy were observed in 6% (2/33) of the patients with generalized lipodystrophy tested. Adverse events reported in these two patients included severe infections and worsening of metabolic control (increases in HbA1c and/or triglycerides). Test for anti-metreleptin antibodies with neutralizing activity in patients who develop severe infections or show signs suspicious for loss of MYALEPT efficacy during treatment. Contact AstraZeneca at 1-866-216-1526 for testing of clinical samples. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. The immunogenicity assays utilized in clinical trials lacked sensitivity, resulting in potential underestimation of the number of samples positive for anti-metreleptin antibodies with neutralizing activity. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to metreleptin with the incidence of antibodies to other products may be misleading. 7 DRUG INTERACTIONS No formal drug interaction studies were performed. Leptin is a cytokine and may have the potential to alter the formation of cytochrome P450 (CYP450) enzymes. This should be taken into account when prescribing concomitant drugs metabolized by CYP450 (e.g., oral contraceptives and drugs with a narrow therapeutic index). The effect of metreleptin on CYP450 enzymes may be clinically relevant for CYP450 substrates with narrow therapeutic index, where the dose is individually adjusted. Upon initiation or discontinuation of MYALEPT, in patients being treated with these types of agents, therapeutic monitoring of effect (e.g., warfarin) or drug concentration (e.g., cyclosporine or theophylline) should be performed and the individual dose of the agent adjusted as needed. 8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Pregnancy Category C There is a program that monitors outcomes in women exposed to MYALEPT during pregnancy. Women who become pregnant during MYALEPT treatment are encouraged to enroll. Patients or their physicians should call 1-855-6MYALEPT to enroll. Risk Summary There are no adequate and well-controlled studies of MYALEPT in pregnant women. All pregnancies, regardless of drug exposure, have a background rate of 2% to 4% for major malformations and 15% to 20% for pregnancy loss. In a pre- and postnatal development study in mice, administration of metreleptin caused prolonged gestation and dystocia resulting in maternal death during parturition and lower survival of offspring in the immediate postnatal period at doses starting approximately at the maximum recommended clinical dose. Because animal reproduction studies are not always predictive of human response, MYALEPT should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Clinical Considerations Disease-Associated Maternal and Fetal Risk The contribution of MYALEPT to obstetrical risks and complications is unknown compared with those already documented in the lipodystrophy patient population (e.g., gestational diabetes, macrosomia, eclampsia, intrauterine growth retardation, intrauterine death, and miscarriage). Labor and Delivery The effects of MYALEPT on labor and delivery in pregnant women are unknown. In an in vitro study of human myometrial tissue exposed to a recombinant leptin, human uterine contractility was inhibited. Furthermore, prolonged gestation and dystocia were observed in animal studies with metreleptin (see below). Animal Data Metreleptin administered to pregnant mice during the period of organogenesis was not teratogenic at doses ranging between 7- and 15-fold the maximum recommended clinical dose, based on body surface area of a 20- and 60-kg patient, respectively. In a pre- and postnatal development study in mice, metreleptin administered at doses of 3, 10, and 30 mg/kg (approximately 1-, 5-, and 15-fold the clinical dose for a 60-kg subject, based on body surface area) from gestation day 6 to lactation day 21 caused prolonged gestation and dystocia at all doses, starting at approximately the maximum recommended clinical dose. Prolonged gestation resulted in the death of some females during parturition and lower survival of offspring within the immediate postnatal period. Consistent with metreleptin pharmacology, decreased maternal body weight was observed from gestation throughout lactation at all doses and resulted in reduced weight of offspring at birth, which persisted into adulthood. However, no developmental abnormalities were observed and reproductive performance of the first or second generations was not affected at any dose. Placental transfer of metreleptin into the fetus was low (approximately 1%) following subcutaneous dosing. 8.3 Nursing Mothers It is not known if MYALEPT is present in human milk. Endogenous leptin is present in human milk. Because of the potential for serious adverse reactions (including possible adverse reactions related to passage of anti-metreleptin antibodies) in nursing infants from MYALEPT a decision should be made whether to discontinue nursing or discontinue the drug, taking into account importance of drug to the mother [see Adverse Reactions (6.2) and Nonclinical Toxicology (13.1)]. 8.4 Pediatric Use The MYALEPT study included a total of 35 pediatric patients (73%) with an age range from 1 to 17 years [see Clinical Studies (14.1)]. No clinically meaningful differences were observed in the efficacy and safety of MYALEPT between pediatric and adult patients. MYALEPT contains benzyl alcohol when reconstituted with BWFI. MYALEPT contains no preservative when reconstituted with WFI. Preservative-free WFI is recommended for use in neonates and infants. The preservative benzyl alcohol has been associated with serious adverse events and death, particularly in pediatric patients. The "gasping syndrome" (characterized by central nervous system depression, metabolic acidosis, gasping respirations, and high levels of benzyl alcohol and its metabolites found in the blood and urine) has been associated with benzyl alcohol dosages >99 mg/kg/day in neonates and low-birth weight infants. Additional symptoms may include gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Although normal therapeutic doses of this product deliver amounts of benzyl alcohol that are substantially lower than those reported in association with the "gasping syndrome," the minimum amount of benzyl alcohol at which toxicity may occur is not known. Premature and low-birth-weight infants, as well as patients receiving high dosages, may be more likely to develop toxicity. Practitioners administering this and other medications containing benzyl alcohol should consider the combined daily metabolic load of benzyl alcohol from all sources. When reconstituted with 2.2 mL of BWFI, MYALEPT contains 1.76 mg of benzyl alcohol per mg of metreleptin or 9 mg of benzyl alcohol per mL of reconstituted product. 8.5 Geriatric Use Clinical trials of MYALEPT did not include sufficient numbers of subjects aged 65 and over (n=1) to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. 10 OVERDOSAGE There were no reports of overdose in the lipodystrophy clinical trial program of MYALEPT. In the event of an overdose, patients should be monitored and appropriate supportive treatment be initiated as dictated by the patient’s clinical status. 11 DESCRIPTION MYALEPT (metreleptin) for injection is a recombinant human leptin analog for injection that binds to and activates the leptin receptor. Metreleptin (recombinant methionyl-human leptin) is produced in E. coli and differs from native human leptin by the addition of a methionine residue at its amino terminus. Metreleptin is a 147-amino acid, nonglycosylated, polypeptide with one disulfide bond between Cys-97 and Cys-147 and a molecular weight of approximately 16.15 kDa. MYALEPT is supplied as a sterile, white, solid, lyophilized cake containing 11.3 mg that is reconstituted with 2.2 mL of BWFI or WFI to a final formulation of 5 mg/mL metreleptin for subcutaneous injection. Inactive ingredients are: glutamic acid (1.47 mg/mL), glycine (20 mg/mL), polysorbate 20 (0.1 mg/mL), and sucrose (10 mg/mL), pH 4.25. 12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Adipocytes store lipids to meet the fuel requirements of non-adipose tissues during fasting. In patients with generalized lipodystrophy, the deficiency of adipose tissue leads to hypertriglyceridemia and ectopic deposition of fat in non-adipose tissues such as liver and muscle, contributing to metabolic abnormalities including insulin resistance. Native leptin is a hormone predominantly secreted by adipose tissue that informs the central nervous system of the status of energy stores in the body. In patients with generalized lipodystrophy, leptin deficiency, resulting from the loss of adipose tissue, contributes to excess caloric intake, which exacerbates the metabolic abnormalities. MYALEPT (metreleptin) for injection exerts its function by binding to and activating the human leptin receptor (ObR), which belongs to the Class I cytokine family of receptors that signals through the JAK/STAT transduction pathway. 12.2 Pharmacodynamics Clinical studies in patients with generalized lipodystrophy suggest that MYALEPT increases insulin sensitivity and reduces food intake. Improvements in insulin sensitivity and reductions in food intake are consistent with lower HbA1c, fasting glucose, and fasting triglyceride values that were seen in the MYALEPT clinical trial [see Clinical Studies (14)]. 12.3 Pharmacokinetics There are limited data on the pharmacokinetics of metreleptin in patients with generalized lipodystrophy, and therefore, no formal exposure-response analysis has been performed. It should be noted that the leptin assay measures both endogenous leptin as well as exogenously administered metreleptin. Absorption Peak serum leptin concentration (Cmax) occurred approximately 4.0 to 4.3 hours after subcutaneous administration of single doses ranging from 0.1 to 0.3 mg/kg in healthy subjects. In a supportive trial in lipodystrophy patients, the median Tmax of metreleptin was 4 hours (range: 2 to 8 hours; N=5) following single-dose administration of metreleptin. Distribution In studies of healthy adult subjects, following intravenous administration of metreleptin, leptin volume of distribution was approximately 4 to 5 times plasma volume; volumes (Vz) (mean ± SD) were 370 ± 184 mL/kg, 398 ± 92 mL/kg, and 463 ± 116 mL/kg for 0.3, 1.0, and 3.0 mg/kg/day doses, respectively. Metabolism and Elimination No formal metabolism studies have been conducted with metreleptin. Nonclinical data indicate renal clearance is the major route of metreleptin elimination, with no apparent contribution of systemic metabolism or degradation. Following single subcutaneous doses of 0.01 to 0.3 mg/mL metreleptin in healthy subjects, the half-life was 3.8 to 4.7 hours. The clearance of metreleptin is expected to be delayed in the presence of leptin antibodies [see Adverse Reactions (6.2)]. Drug Interactions No drug interaction studies have been conducted in lipodystrophy patients [see Drug Interactions (7)]. Specific Populations Renal Impairment No formal pharmacokinetic studies were conducted in patients with renal impairment. Nonclinical data indicate renal clearance is the major route of metreleptin elimination, with no apparent contribution of systemic metabolism or degradation. Hence, the pharmacokinetics of metreleptin may be altered in subjects with renal impairment. Hepatic Impairment No formal pharmacokinetic studies were conducted in patients with hepatic impairment. Age, Gender, Race, Body Mass Index Specific clinical studies have not been conducted to assess the effect of age, gender, race, or body mass index on the pharmacokinetics of metreleptin in patients with generalized lipodystrophy. 13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Two-year carcinogenicity studies in rodents have not been conducted with metreleptin. No proliferative or preneoplastic lesions were observed in mice or dogs following treatment up to six months. However, leptin is reported in the literature to promote cell proliferation in vitro and tumor progression in some mouse models of cancer. Metreleptin was not mutagenic in the Ames bacterial mutagenicity assay or clastogenic in an in vitro chromosomal aberration assay in Chinese hamster ovary cells and human peripheral blood lymphocytes. Metreleptin was not mutagenic or clastogenic in an in vivo mouse micronucleus assay. In a fertility study in mice, metreleptin had no adverse effects on mating, fertility, or early embryonic development at doses ranging between 7 and 15 times the maximum recommended clinical dose based on body surface area of a 20- and 60-kg patient, respectively. 14 CLINICAL STUDIES 14.1 Open-Label, Single-Arm Study An open-label, single-arm study evaluated MYALEPT treatment in patients with congenital or acquired generalized lipodystrophy and diabetes mellitus, hypertriglyceridemia, and/or increased fasting insulin. Baseline Disease Characteristics and Demographics Of the 48 patients enrolled, 32 (67%) had congenital generalized lipodystrophy and 16 (33%) had acquired generalized lipodystrophy. Overall, 36 (75%) patients were female, 22 (46%) were Caucasian, 10 (21%) Hispanic, and 9 (19%) Black. The median age at baseline was 15 years (range: 1 - 68 years), with 35 (73%) patients being less than 18 years of age. The median fasting leptin concentration at baseline was 0.7 ng/mL in males (range: 0.3 - 3.3 ng/mL) and 1.0 ng/mL in females (range: 0.3 - 3.3 ng/mL). Treatment Duration and Dosage in the Study The median duration of MYALEPT treatment was 2.7 years (range: 3.6 months - 10.9 years). MYALEPT was administered subcutaneously either once daily or twice daily (in two equal doses). The weighted average daily dose (i.e., the average dose taking into account duration of treatment at different doses) for the 36 patients with baseline body weight greater than 40 kg was 2.6 mg for males and 4.6 mg for females during the first year of treatment, and 3.2 mg for males and 6.3 mg for females over the entire study period. For the 12 patients with baseline body weight less than 40 kg, the weighted average daily dose was 0.06 to 0.11 mg/kg (0.8-4.3 mg) over the entire study period. Efficacy Results At baseline, 37 (77%) patients had HbA1c values of 7% or greater, 19 (40%) had HbA1c values of 9% or greater, 33 (69%) had fasting plasma glucose values of 126 mg/dL or greater, 17 (35%) had fasting triglyceride values of 500 mg/dL or greater, and 11 (23%) had fasting triglyceride values of 1000 mg/dL or greater. Patients treated with MYALEPT had mean/median reductions in HbA1c, fasting glucose, and triglycerides at 1 year (Table 3). The changes in HbA1c, fasting glucose, and triglycerides observed at Month 4 were similar to those at 1 year. Concomitant antihyperglycemic and lipid-altering medication dosage regimens were not held constant during the study; for example, some patients treated with insulin had their dosage increased and others had large reductions or discontinuation of insulin. Table 3: Results in an Open-Label, Single-Arm Study in Patients with Generalized Lipodystrophy Treated with MYALEPT (N=48)
Among 28 patients with generalized lipodystrophy who had a baseline HbA1c 7% or greater and data available at Month 12, the mean (SD) baseline HbA1c was 9.3 (1.5%) and the mean reduction in HbA1c at Month 12 was 2.4%. Among 12 patients with generalized lipodystrophy who had a baseline triglyceride level 500 mg/dL or greater and data available at Month 12, the median baseline triglyceride level was 1527 mg/dL and the median reduction in triglycerides at Month 12 was 1117 mg/dL. 16 HOW SUPPLIED/STORAGE AND HANDLING 16.1 How Supplied • MYALEPT (metreleptin) for injection for subcutaneous administration is supplied in a single carton containing one vial for reconstitution (NDC 66780-310-01). • Each vial contains 11.3 mg metreleptin (as a sterile, white, solid, lyophilized cake) to deliver 5 mg per mL of metreleptin when reconstituted with 2.2 mL of BWFI or WFI. 16.2 Storage and Handling • MYALEPT should be stored in the refrigerator at 36°F to 46°F (2°C to 8°C) and protected from light until preparing for use. Keep MYALEPT vials in the carton when not in use. • MYALEPT should not be used past the expiration date. • Do not freeze MYALEPT. • Do not use if the white lyophilized cake is discolored. • Use with BWFI: when MYALEPT is reconstituted with BWFI, the vial can be used for multiple doses within 3 days when stored in the refrigerator at 36°F to 46°F (2°C to 8°C) and protected from light. • Use with WFI: when MYALEPT is reconstituted with WFI, the vial can be used for a single dose should be administered immediately. Unused reconstituted solution cannot be saved for later use and should be discarded. • After reconstitution, the vials should not be frozen (below 0°C) or shaken vigorously. If the reconstituted product is inadvertently frozen, it should be thrown away. • After reconstitution, the mixture should be clear and colorless. Do not use if visible particulates are present in the solution. • Keep out of the reach of children. 17 PATIENT COUNSELING INFORMATION See FDA-approved Patient Labeling (Medication Guide). Risk of Neutralizing Antibodies Advise patients that neutralizing antibodies may result in loss in activity of endogenous leptin or loss of efficacy of MYALEPT. Advise patients on symptoms or signs that would warrant antibody testing [see Warnings and Precautions (5.1) and Adverse Reactions (6.2)]. Risk of Lymphoma Advise patients that lymphoma has been reported in patients both treated and not treated with MYALEPT. Advise patients on symptoms or signs that indicate changes in hematologic status and the importance of routine laboratory assessments and physician monitoring [see Warnings and Precautions (5.2)]. Risk of Hypoglycemia Advise patients that the risk of hypoglycemia is increased when MYALEPT is used in combination with insulin or an insulin secretagogue (e.g., sulfonylurea). Explain the symptoms, treatment, and conditions that predispose to development of hypoglycemia to the patient. Advise patients who are taking concomitant insulin, especially those on high doses, or an insulin secretagogue, to closely monitor blood glucose. Hypoglycemia management should be reviewed and reinforced when initiating MYALEPT therapy, particularly when concomitantly administered with insulin or an insulin secretagogue [see Warnings and Precautions (5.4)]. Risk of Autoimmune Disease Advise patients that worsening of autoimmune disease has been reported during the clinical study of MYALEPT. Advise patients with a history of autoimmune disease on symptoms or signs that indicate exacerbation of underlying autoimmune disease and the importance of routine laboratory assessments and physician monitoring [see Warnings and Precautions (5.5)]. Risk of Hypersensitivity Reactions Inform patients that hypersensitivity reactions have been reported during use of MYALEPT. If symptoms of hypersensitivity reactions occur, patients should seek medical advice [see Warnings and Precautions (5.6)]. Nursing Mothers Advise nursing mothers that breastfeeding is not recommended with MYALEPT use [see Use in Specific Populations (8.3)]. Instructions • Inform patients that each vial of MYALEPT requires reconstitution with BWFI or preservative-free WFI, and administration as subcutaneous injection using a syringe and needle. Injections can be given at any time of the day, with or without meals. • Patients and caregivers should receive proper training in how to prepare and administer the correct dose of MYALEPT prior to self-administration. The first dose of MYALEPT should be administered by the patient or caregiver under the supervision of a qualified healthcare professional. • Advise patients on injection technique, dosing regimen, and the importance of proper storage of MYALEPT. Care should be taken to avoid intramuscular injection, especially in patients with minimal subcutaneous adipose tissue. • Advise patients to read the Instructions for Use for complete administration instructions. The MYALEPT Medication Guide and Instructions for Use should be reviewed before starting therapy and each time the prescription is refilled. • When discontinuing MYALEPT in patients with a history of pancreatitis and/or severe hypertriglyceridemia, instruct patients to taper their dose over a one-week period. Advise patients that additional monitoring of triglyceride levels and possible initiation or dose adjustment of lipid-lowering medications may be considered [see Dosage and Administration (2.5)]. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||