1。对产品的名称
ZIBOR 3500 IU反Xa/0.2注射毫升溶液中预充式注射器
2。定性和定量组成
Bemiparin钠:3500 IU(抗Xa因子*)每0.2毫升的预填充注射器(相当于17500 IU(antiFactor XA *)每毫升注射液)
效力在国际抗Xa因子活性单位(IU的第一届国际低分子量肝素参考标准)
辅料的质量,见6.1
3。剂型
预充注射器注入解决方案。
(无色或微黄色,清晰的解决方案,无可见颗粒)
4。临床详情
4.1适应症
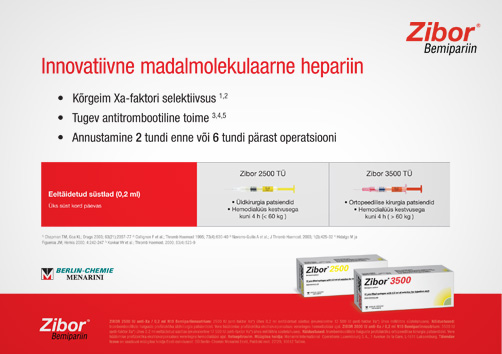
在接受骨科手术的患者血栓栓塞性疾病的预防。
防止在体外循环血液透析过程中凝血。
4.2 Posology管理方法
警告:不同低分子量肝素不一定是等价的。因此,遵守给药方案和具体的使用方法,这些药用产品是必需的。
成人:
骨科手术的静脉血栓栓塞的高风险:
在当天的手术,3500 IU抗Xa是由皮下的路线,前2小时或6小时的手术后管理。在随后的日子里,3500 IU抗Xa SC是要管理的每24个小时。
预防性治疗后,必须根据医生的意见,在危险期,或直到病人是动员。作为一般规则,它认为有必要保持至少7预防性治疗 - 外科手术后10天,直到血栓栓塞性疾病的风险下降。
在血液透析过程中的体外循环凝血的预防:
对于患者接受血液透析不再重复,持续时间超过4小时无出血的危险性,预防在体外循环血液透析过程中凝固是在单剂量的推注的形式注入动脉行的开头透析会议。对于体重不到60公斤的患者,剂量将是2500国际单位,而对于体重超过60公斤的患者,剂量为3500 IU。
儿童:bemiparin在儿童使用的安全性和疗效尚未确定,因此不建议使用儿童。
老年人:无需调整剂量。
肾和肝功能不全:有足够的数据来建议在本组患者的bemiparin的剂量调整。
管理方法。皮下注射技术:
预充式注射器可以立即使用,不得清除前皮下注射。当ZIBOR皮下注射,注射应在皮下细胞组织的腹部外侧或后外侧腰,左,右两侧交替。应完全插入针,垂直和切线,拇指和食指之间举行了皮褶厚,皮褶应在整个注射举行。不要揉搓注射部位。
4.3禁忌
bemiparin钠,肝素或猪源物质过敏。
证实或怀疑有免疫介导的肝素诱导血小板减少症(HIT)的历史记录(见4.4:特别警告和使用时的注意事项)。
积极出血或出血的止血减值的风险增加。
肝脏和胰腺功能严重受损
对中枢神经系统和操作受伤,眼睛和耳朵
弥散性血管内凝血(DIC)的归属于肝素诱导的血小板减少症。
急性细菌性心内膜炎和心内膜炎lenta
器质性病变出血的高风险(如活动性溃疡,haemorragic中风,脑动脉瘤或脑肿瘤)。
4.4特别警告和使用时的注意事项
不要肌肉注射管理。
由于风险管理bemiparin血肿在其他药物的肌肉注射,应避免
在肝或肾功能衰竭,动脉高血压失控,胃十二指肠球部溃疡病,血小板减少,肾结石和/或urethrolithiasis,脉络膜和视网膜血管疾病史,或任何其他器质性病变,出血等并发症的风险增加患者,应小心或在发生脊髓或硬膜外麻醉和/或腰椎穿刺的患者。
Bemiparin,像其他低分子肝素可以抑制肾上腺分泌醛固酮,导致高钾血症,特别是在如糖尿病,慢性肾功能衰竭,预先存在的代谢性酸中毒,提高血浆钾或服用保钾药物的患者。出现高钾血症的风险增加的治疗时间,但通常是可逆的。应测量患者血清电解质开始bemiparin治疗前的风险,并定期监测以后,特别是如果治疗是延长超过7天左右。
偶尔有轻微的瞬态血小板减少症(I型)与肝素之间的10万个/ mm3和15万个/ mm3,由于暂时的血小板活化的血小板计数在治疗开始已被观察到(见4.8不良反应)。作为一项规则,无并发症发生,因此可以继续治疗。
抗体介导的严重的血小板减少与血小板计数明显低于10万个/ mm3(II型)在极少数情况下已被观察到(见4.8不良反应)。这种效应通常发生在治疗开始后的5至21天;患者肝素诱导的血小板减少症,这迟早可能发生的历史。
血小板计数建议之前bemiparin管理,在治疗的第一天,然后定期3至4天,并在治疗结束与bemiparin。在实践中,治疗必须立即停止和启动替代疗法如果观察血小板计数显着减少(30%至50%),与bemiparin存在抗血小板抗体在体外试验阳性或未知的结果相关或其他低分子肝素和/或肝素。
与其他肝素,皮肤坏死,有时减少性紫癜或痛苦的红斑黑斑之前,已将有关个案呈报bemiparin(见4.8不良反应)。在这种情况下,应立即停止治疗。
在接受硬膜外麻醉或腰麻或腰穿的患者,预防性使用肝素可能很少与硬膜外或脊髓血肿,导致长期或永久瘫痪(见4.8不良反应)。风险是影响止血的药物,如非类固醇消炎药(NSAIDs),血小板抑制剂或抗凝血剂同时使用,增加使用麻醉硬膜外或脊髓导管(见4.5:与其他医药产品和其他的相互作用互动的形式),以及由外伤或反复穿刺。
当到达最后在预防剂量肝素和安置或清除硬膜外或脊髓导管之间的间隔决定,产品的特点和病人的个人资料,应予以考虑。 bemiparin随后剂量不应采取的地方,直到至少有四个小时后拔除导尿管。随后的剂量应推迟到完成手术过程。
如果医生决定管理抗凝治疗在硬膜外麻醉或腰麻,高度警惕和频繁的监测必须行使的情况下,检测到任何神经受损的症状和体征,如背痛,感觉和运动障碍(麻木和弱点在较低,四肢)和肠道或膀胱功能障碍。护士应进行培训,以检测这些症状和体征。应指示患者立即告知护士或临床医生,如果他们的经验这些症状。
如果硬膜外或脊髓血肿的症状或体征,应开始怀疑,紧急的诊断和治疗,包括髓减压。
4.5与其他医药产品和其他形式的互动的相互作用
与其他药用产品的Bemiparin互动都没有受到调查,本节提供的资料是从的数据从其他低分子量肝素的
随之而来的管理bemiparin及以下的药用产品是不可取的:
维生素K拮抗剂和其他抗凝血剂,乙酰水杨酸和其他水杨酸和非甾体抗炎药,噻氯匹定,氯吡格雷和其他血小板抑制剂全身糖皮质激素和葡聚糖。
所有这些药物通过干扰凝血和/或血小板功能的作用,增加出血的危险增加的药理bemiparin作用。
如果无法避免的组合,它应采用谨慎的临床和实验室监测。
医药产品,增加血清钾浓度只应特别小心的医疗监督下随之而来
肝素静脉注射硝酸甘油(这可能会导致疗效下降)之间的相互作用不能排除bemiparin。
4.6怀孕和哺乳
妊娠:动物研究并没有显示出任何与bemiparin使用(见5.3:临床前安全性数据)的致畸作用的证据。 bemiparin,暴露怀孕没有临床数据。因此,应谨慎处方时孕妇。 bemiparin是否穿过胎盘屏障,它是未知的。
哺乳期:bemiparin是否进入乳汁传递信息不足。因此,它是哺乳期的母亲收到ZIBOR必要,他们应尽量避免喂哺母乳
4.7驾驶和使用机器能力的影响
Bemiparin有没有影响的能力来驱动,并使用精密或危险机械。
4.8不良反应
最常见的不良反应是血肿和/或有瘀斑,注射部位,发生在约15%的患者接受ZIBOR。
一直伴随着长期的肝素治疗骨质疏松症。
频率的AES报告bemiparin类似报告与其他低分子肝素如下:
非常常见(> 1 / 10):
- 在注射部位的瘀血
常见(> 1 / 100,<1 / 10):
- 血肿和注射部位疼痛。
- 出血并发症(皮肤,粘膜,伤口,肠道,泌尿生殖道)。
- 轻微和短暂的海拔转氨酶(ASAT,ALAT)和γ- GT水平。
不常见(> 1 / 1000,<1 / 100):
- 皮肤过敏反应(荨麻疹,瘙痒)
- 轻微和短暂的血小板减少症(I型)(见4.4:特别警告和使用时的注意事项)。
罕见(<1 / 1000):
- 过敏性反应(恶心,呕吐,发烧,呼吸困难,支气管痉挛,声门水肿,低血压,荨麻疹,瘙痒)。
- 严重的血小板减少症(II型)(见4.4:特别警告和使用时的注意事项)。
- 在注射部位的皮肤坏死(见4.4:特别警告和使用时的注意事项)。
- 硬膜外和椎管内血肿,硬膜外麻醉或腰麻和腰穿。这些血肿造成了不同程度的神经功能损害,包括长期或永久瘫痪(见4.4:特别警告和使用时的注意事项)。
4.9过量
出血是过量的主要症状。 Bemiparin应停止根据出血的严重程度和血栓形成的危险。
轻微出血很少需要特定的治疗。在重大出血的情况下,政府可能需要硫酸鱼精蛋白。
瓦解与鱼精蛋白硫酸盐bemiparin已在体外研究和体内,目的是观察抗Xa活性的减少和APTT的影响。鱼精蛋白硫酸盐发挥抗Xa活性的部分减少为2小时静脉给药后,剂量为1.4毫克每100 IU抗Xa管理鱼精蛋白硫酸盐。
5。药理特性
5.1药效学特性
药物治疗组:抗血栓剂,肝素组。 ATC代码B01AB12。
Bemiparin钠是从猪肠道黏膜肝素钠解聚获得一个低分子量肝素。其平均分子量(MW)的大约3600道尔顿。连锁与分子量低于2000道尔顿的比例不到35%。链,从2000到6000道尔顿分子量的比例范围50-75%之间。与分子量大于6000道尔顿更高链的百分比小于15%。
80和120之间的抗Xa活性范围的抗Xa IU每毫克和抗IIa抗IIa IU干物质计算每毫克,5和20之间的活动范围。 anti-Xa/anti-IIa的比例大约为8。
在动物实验模型,bemiparin抗栓活性和中度出血效果。
在人类中,bemiparin已经证实其抗血栓活性和,在推荐剂量,它不显著延长全球凝血测试。
5.2药代动力学性质
bemiparin的药代动力学性质已确定通过测量血浆抗Xa活性使用amydolitic方法,它是参考世卫组织的第一届国际低分子量肝素参考标准(NIBSC)。
吸收和消除过程中遵循的一阶线性动力学。
吸收:Bemiparin钠吸收迅速,皮下注射和生物利用度估计为96%。最高血浆抗Xa在2500 IU和3500 IU预防剂量效应发生的bemiparin皮下注射后的2至3小时,高峰期的活动,分别达到0.34 + 0.08和0.45 +0.07 IU anti-Xa/ml秩序。没有检测到这些剂量的抗IIa活性。最高血浆抗Xa 5000 IU治疗剂量的影响,出现7500万国际单位,IU和12500 IU的bemiparin皮下注射后3至4小时,达到峰值在0.54为了活动+ 0.06,1.22 ± 0.27,1.42 + 0.19和2.03 +0.25 IU anti-Xa/ml,分别。抗IIa 0.01 IU / ml的活动是在7500万国际单位,IU和12500 IU剂量检测。
消除:在2500 IU到12,500国际单位的剂量范围内管理Bemiparin约5至6小时的半衰期,因此,应每天给药一次。
目前有关于血浆蛋白结合,代谢和排泄人类bemiparin无可用数据。
5.3临床前安全性数据
bemiparin的临床前数据表明没有特殊危害人类基于传统安全药理学,单一和重复剂量毒性遗传毒性和生殖毒性研究。
急性和重复剂量的毒性研究,在动物皮下bemiparin管理人士透露改建组成基本上是可逆的,在注射部位的剂量依赖性haemorragic病变。这些被认为是导致夸张的药理活性。
在怀孕大鼠和家兔bemiparin怀孕6和18天之间,生殖毒性研究,无死亡记录在与bemiparin治疗的女性。记录的主要临床体征皮下血肿是由于药理作用的测试项目。无治疗相关的胚胎效果既无外债,骨骼和/或内脏的变化,记录在检查胎儿
6。医药详情
6.1辅料的名单
水为注射
6.2不兼容的问题
与其他任何注射或输液ZIBOR不应混为一谈。
6.3保质期
2年。
第一次打开后,应立即使用ZIBOR
6.4存储的特别措施
不要储存30 ° C以上,不要冷冻
6.5自然和容器的内容
0.2毫升溶液中预充注射器(I型玻璃)与柱塞杆(聚丙烯),橡胶活塞瓶塞(氯化)和注射针(不锈钢)。包2,6,10,30和100个注射器。
请注意:并非所有的包装规格可销售
6.6处理和其他处理的特别注意事项
单剂量容器。丢弃任何未使用的的内容。不要使用保护包,如果是打开或损坏。无色透明或微黄色的解决方案,无可见颗粒,应使用。任何未使用的产品和注射针头应按照当地的要求处置。
7。上市许可持有人
ROVI成像S.L.
鲁菲诺冈萨雷斯,50
马德里 - 西班牙
8。营销授权号(S)
ZIBOR 3500 IU,注册号:30417/0002
9。第一授权/授权续期日期
2002年3月10日
10。修订的文本日期
2007年6月
1. NAME OF THE MEDICINAL PRODUCT
ZIBOR 3,500 IU anti Xa/0.2 ml solution for injection in pre-filled syringes
|
Bemiparin sodium: 3500 IU (anti Factor Xa*) per 0.2 ml pre-filled syringe (equivalent to 17500 IU (antiFactor Xa*) per millilitre solution for injection) Potency is described in International anti-Factor Xa activity units (IU) of the 1st International Low Molecular Weight Heparin Reference Standard For excipients, see 6.1 |
|
Solution for injection in pre-filled syringe. (Colourless or slightly yellowish, clear solution, free of visible particles) |
|
Prevention of thromboembolic disease in patients undergoing orthopaedic surgery. Prevention of clotting in the extracorporeal circuit during haemodialysis. |
Adults: Orthopaedic surgery with high risk of venous thromboembolism: On the day of the surgical procedure, 3,500 IU anti-Xa is to be administered by subcutaneous route, 2 hours before or 6 hours after surgery. On subsequent days, 3,500 IU anti-Xa sc is to be administered every 24 hours. Prophylactic treatment must be followed in accordance with the physician's opinion during the period of risk or until the patient is mobilised. As a general rule, it is considered necessary to maintain prophylactic treatment for at least 7 – 10 days after the surgical procedure and until the risk of thromboembolic disease has decreased.
Prevention of clotting in the extracorporeal circuit during haemodialysis: For patients undergoing repeated haemodialysis of no longer than 4 hours in duration and with no risk of bleeding, the prevention of clotting in the extracorporeal circuit during haemodialysis is obtained by injecting a single dose in the form of bolus into the arterial line at the beginning of the dialysis session. For patients weighing less than 60 kg, the dose will be 2,500 IU, whereas for patients weighing more than 60 kg, the dose will be 3,500 IU. Children: The safety and efficacy of the use of bemiparin in children has not been established, therefore the usage in children is not recommended. Elderly: No dose adjustment required. Renal and hepatic impairment: There are insufficient data to recommend a dose adjustment of bemiparin in this group of patients.
Method of administration. Subcutaneous injection technique: The pre-filled syringes are ready for immediate use and must not be purged before the subcutaneous injection. When ZIBOR is administered subcutaneously, the injection should be given in the subcutaneous cell tissue of the anterolateral or posterolateral abdominal waist, alternately on the left and right sides. The needle should be fully inserted, perpendicularly and not tangentially, into the thick part of a skin fold held between the thumb and the forefinger; the skin fold should be held throughout the whole injection. Do not rub the injection site. |
|
Hypersensitivity to bemiparin sodium, heparin or substances derived from pigs. History of confirmed or suspected immunologically mediated heparin induced thrombocytopenia (HIT) (see 4.4: Special warnings and precautions for use). Active haemorrhage or increased risk of bleeding due to impairment of haemostasis. Severe impairment of liver and pancreas function Injuries to and operations on the central nervous system, eyes and ears Disseminated Intravascular Coagulation (DIC) attributable to heparin-induced thrombocytopenia. Acute bacterial endocarditis and endocarditis lenta Organic lesion with high risk of bleeding (e.g. active peptic ulcer, haemorragic stroke, cerebral aneurysm or cerebral neoplasms). |
|
Do not administer by the intramuscular route. Due to the risk of haematoma during bemiparin administration the intramuscular injection of other agents should be avoided Caution should be exercised in patients with liver or renal failure, uncontrolled arterial hypertension, history of gastro-duodenal ulcer disease, thrombocytopenia, nephrolithiasis and/or urethrolithiasis, choroid and retinal vascular disease, or any other organic lesion with an increased risk of bleeding complications, or in patients undergoing spinal or epidural anaesthesia and/or lumbar puncture. Bemiparin, like other LMWHs, can suppress adrenal secretion of aldosterone leading to hyperkalaemia, particularly in patients such as those with diabetes mellitus, chronic renal failure, pre-existing metabolic acidosis, a raised plasma potassium or taking potassium sparing drugs. The risk of hyperkalaemia appears to increase with the duration of therapy but is usually reversible. Serum electrolytes should be measured in patients at risk before starting bemiparin therapy and monitored regularly thereafter particularly if treatment is prolonged beyond about 7 days. Occasionally a mild transient thrombocytopenia (type I) at the beginning of therapy with heparin with platelet counts between 100,000/mm3 and 150,000/mm3 due to temporary platelet activation has been observed (see 4.8: Undesirable effects). As a rule, no complications occur, therefore treatment can be continued. In rare cases antibody-mediated severe thrombocytopenia (type II) with platelet counts clearly below 100,000/mm3 has been observed (see 4.8: Undesirable effects). This effect usually occurs within 5 to 21 days after the beginning of treatment; in patients with a history of heparin-induced thrombocytopenia this may occur sooner. Platelet counts are recommended before administration of bemiparin, on the first day of therapy and then regularly 3 to 4 days and at the end of therapy with bemiparin. In practice, treatment must be discontinued immediately and an alternative therapy initiated if a significantly reduced platelet count is observed (30 to 50 %) ,associated with positive or unknown results of in-vitro tests for anti-platelet antibody in the presence of bemiparin or other LMWHs and /or heparins. As with other heparins, cases of cutaneous necrosis, sometimes preceded by purpura or painful erythematous blotches have been reported with bemiparin (see 4.8: Undesirable effects). In such cases, treatment should be discontinued immediately. In patients undergoing epidural or spinal anaesthesia or lumbar puncture, the prophylactic use of heparin may very rarely be associated with epidural or spinal haematoma, resulting in prolonged or permanent paralysis (see 4.8: Undesirable effects). The risk is increased by the use of an epidural or spinal catheter for anaesthesia, by the concomitant use of drugs affecting haemostasis such as nonsteroidal anti-inflammatory drugs (NSAIDs), platelet inhibitors or anticoagulants (see 4.5: Interaction with other medicinal products and other forms of interaction), and by traumatic or repeated puncture. When reaching a decision as to the interval between the last heparin administration at prophylactic doses and the placement or removal of an epidural or spinal catheter, the product characteristics and the patient profile should be taken into account. The subsequent dose of bemiparin should not take place until at least four hours after removal of the catheter. The subsequent dose should be delayed until the surgical procedure is completed. Should a physician decide to administer anticoagulation treatment in the context of epidural or spinal anaesthesia, extreme vigilance and frequent monitoring must be exercised to detect any signs and symptoms of neurological impairment, such as back pain, sensory and motor deficits (numbness and weakness in lower limbs) and bowel or bladder dysfunction. Nurses should be trained to detect such signs and symptoms. Patients should be instructed to inform a nurse or a clinician immediately if they experience any of these symptoms. If signs or symptoms of epidural or spinal haematoma are suspected, urgent diagnosis and treatment including medullary decompression should be initiated. |
|
Bemiparin interactions with other medicinal products have not been investigated and the information given on this section is derived from data available from other LMWH The concomitant administration of bemiparin and the following medicinal products is not advisable: Vitamin K antagonists and other anticoagulants, acetyl salicylic acid and other salicylates and NSAIDs, ticlopidine, clopidogrel and other platelet inhibitors systemic glucocorticoids and dextran . All these drugs increase the pharmacological effect of bemiparin by interfering with its action on coagulation and/or platelet function and increasing the risk of bleeding. If the combination cannot be avoided, it should be used with careful clinical and laboratory monitoring. Medicinal products that increase the serum potassium concentration should only be taken concomitantly under especially careful medical supervision Interaction of heparin with intravenous nitroglycerine (which can result in a decrease in efficacy) cannot be ruled out for bemiparin. |
|
Pregnancy: Animal studies have not shown any evidence of teratogenic effects with the use of bemiparin (see 5.3: Preclinical safety data). For bemiparin, no clinical data on exposed pregnancies are available. Therefore, caution should be exercised when prescribing to pregnant women. It is unknown whether bemiparin crosses placental barrier. Lactation: Insufficient information is available as to whether bemiparin passes into breast milk. Therefore, where it is necessary for lactating mothers to receive ZIBOR, they should be advised to avoid breast-feeding |
|
Bemiparin has no influence on the ability to drive and use precision or dangerous machinery. |
|
The most commonly reported adverse reaction is haematoma and/or ecchymosis at the injection site, occurring in approximately 15 % of patients receiving ZIBOR. Osteoporosis has been associated with long-term heparin treatment. The frequency of AEs reported with bemiparin are similar to those reported with other LMWHs and is as follows: Very common ( >1/10): - Ecchymosis at injection site Common (>1/100, <1/10): - Haematoma and pain at injection site. - Bleeding complications (skin, mucous membranes, wounds, gastro-intestinal tract, urogenital tract). - Mild and transient elevations of transaminases (ASAT, ALAT) and gamma-GT levels. Uncommon (>1/1000, <1/100): - Cutaneous allergic reactions (urticaria, pruritus) - Mild and transient thrombocytopenia (type I) (see 4.4: Special warnings and precautions for use). Rare (<1/1000): - Anaphylactic reactions (nausea, vomiting, fever, dyspnoea, bronchospasm, glottis oedema, hypotension, urticaria, pruritus). - Severe thrombocytopenia (type II) (see 4.4: Special warnings and precautions for use). - Cutaneous necrosis at the injection site (see 4.4: Special warnings and precautions for use). - Epidural and spinal haematoma following epidural or spinal anaesthesia and lumbar puncture. These haematomas have caused various degrees of neurological impairment, including prolonged or permanent paralysis (see 4.4: Special warnings and precautions for use). |
|
Bleeding is the main symptom of overdose. Bemiparin should be discontinued depending on the severity of the haemorrhage and the risk of thrombosis. Minor haemorrhages rarely need specific treatment. In case of major haemorrhages, administration of protamine sulphate may be needed. The neutralisation of bemiparin with protamine sulphate has been studied in-vitro and in-vivo, with the aim of observing the reduction of anti-Xa activity and the effect on the APTT. Protamine sulphate exerts a partial decrease on anti-Xa activity for 2 hours after its intravenous administration, at a dose of 1.4 mg of protamine sulphate each 100 IU anti-Xa administered. |
|
Pharmacotherapeutic group: antithrombotic agent, heparin group. ATC code B01AB12. Bemiparin sodium is a LMWH obtained by depolymerization of heparin sodium from porcine intestinal mucosa. Its mean molecular weight (MW) is approximately 3,600 daltons. The percentage of chains with MW lower than 2,000 daltons is less than 35%. The percentage of chains with MW from 2,000 to 6,000 daltons ranges between 50-75%. The percentage of chains with MW higher than 6,000 daltons is less than 15%. The anti-Xa activity ranges between 80 and 120 anti-Xa IU per mg and the anti-IIa activity ranges between 5 and 20 anti-IIa IU per mg, calculated in relation to dry matter. The anti-Xa/anti-IIa ratio is approximately 8. In animal experiment models, bemiparin has shown antithrombotic activity and moderate haemorrhagic effect. In humans, bemiparin has confirmed its antithrombotic activity and, at the recommended doses, it does not significantly prolong global clotting tests. |
|
The pharmacokinetic properties of bemiparin have been determined by measuring the plasma anti-Xa activity using the amydolitic method; it is based on reference to the W.H.O. First International Low Molecular Weight Heparin Reference Standard (NIBSC). The absorption and elimination processes follow a linear kinetic of the 1st order. Absorption: Bemiparin sodium is rapidly absorbed following subcutaneous injection and the bioavailability is estimated to be 96%. The maximum plasma anti-Xa effect at prophylactic doses of 2,500 IU and 3,500 IU occurs 2 to 3 hours after subcutaneous injection of bemiparin, reaching peak activities in the order of 0.34 + 0.08 and 0.45 + 0.07 IU anti-Xa/ml, respectively. Anti-IIa activity was not detected at these doses. The maximum plasma anti-Xa effect at treatment doses of 5,000 IU, 7,500 IU, 10,000 IU and 12,500 IU occurs 3 to 4 hours after subcutaneous injection of bemiparin, reaching peak activities in the order of 0.54 + 0.06, 1.22 + 0.27, 1.42 + 0.19 and 2.03 + 0.25 IU anti-Xa/ml, respectively. Anti-IIa activity of 0.01 IU/ ml was detected at doses of 7,500 IU, 10,000 IU and 12,500 IU. Elimination: Bemiparin administered in the dose range of 2,500 IU to 12,500 IU has an approximate half-life of between 5 and 6 hours, and should therefore be administered once daily. There are currently no data available with regards to plasma protein binding, metabolism and excretion of bemiparin in humans. |
|
Preclinical data for bemiparin reveal no special hazard for humans based on conventional studies of safety pharmacology, single and repeated dose toxicity genotoxicity and reproduction toxicity. Acute and repeated dose toxicity studies following subcutaneous administration of bemiparin in animals have revealed alterations consisting essentially in reversible, dose-dependent haemorragic lesions at the injection site. These were considered to result from exaggerated pharmacological activity. In the studies of reproductive toxicity performed with bemiparin in pregnant rats and rabbits, between days 6 and 18 of the pregnancy, no mortality was recorded among the females treated with bemiparin. The main clinical signs recorded were subcutaneous haematomas that were attributable to a pharmacological effect of the test item. No treatment-related embryotoxic effect neither external, skeletal and/or visceral alterations were recorded in the examination of fetuses |
|
Water for injections |
|
ZIBOR should not be mixed with any other injections or infusions. |
|
2 years. After first opening,ZIBOR should be used immediately |
|
Do not store above 30º C. Do not freeze |
|
0.2 ml solution in pre-filled syringe (Type I glass) with a plunger rod (polypropylene), rubber plunger stopper (chlorobutyl) and injection needle (stainless steel). Packs of 2, 6, 10, 30 and 100 syringes. Note: Not all pack sizes may be marketed |
|
Single-dose container. Discard any unused content. Do not use if the protective package is opened or damaged. Only clear and colourless or slightly yellowish solutions, free of visible particles, should be used. Any unused product and injection needles should be disposed of in accordance with local requirements. |
|
ROVI IMAGING S.L. Rufino González, 50 28037 MADRID – SPAIN |
|
ZIBOR 3,500 IU Registration number: 30417/0002 |
|
10 March 2002 |
|
June 2007 |




