|
【药品名称】克拉屈滨注射液
【英文或拉丁名】Cladribine Injection
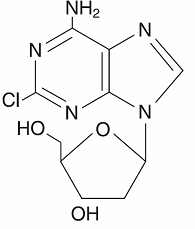
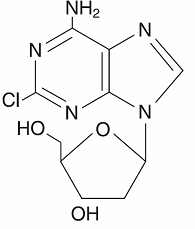
【化学名】2-氯-6-氨基-9-(2-脱氧-β-D-赤型-呋喃戊糖基)嘌呤
【性状】本品为无色或几乎无色的澄明液体。
【药理毒理】
药理作用:
克拉屈滨的抑瘤活性与脱氧胞苷激酶和脱氧核苷酸激酶活性有关。它主要以被动转运进入细胞,在细胞内被脱氧胞苷激酶磷酸化,转化为克拉屈滨三磷酸,掺合到DNA分子中,妨碍DNA断裂后的修复作用,造成NAD和ATP的耗竭,破坏细胞代谢,影响细胞的DNA合成。因此本品对分化或静止期的淋巴细胞和单核细胞均有抑制DNA合成和修复的作用。
毒理研究:
遗传毒性:本品可造成DNA损失,引起哺乳动物细胞DNA链的断裂。本品可进入到人淋巴白细胞。在体外的Ames试验和中国仓鼠细胞染色体畸变试验中和体内的小鼠骨髓微核试验中,本品显示为DNA的断裂剂。
生殖毒性:猕猴静脉给药,本品可引起精子细胞的生成抑制,但对人体生育力的影响不清楚。本品属妊娠D级的药品。
致癌性:未进行本品的动物致癌试验研究,但根据遗传毒性研究结果不排除本品的致癌性可能。
【药代动力学】
尚缺乏克拉屈滨按目前临床推荐剂量用药时的中国人药代动力学资料。
国外一项临床研究中入选肾功能正常的毛细胞白血病患者17名,按克拉屈滨0.09mg/kg/d的剂量连续静滴7日以上,测得平均稳态浓度为5.7ng/ml,总清除率为663.5ml/kg/h。对毛细胞白血病患者而言,本品的血清浓度和最终临床结果间未建立相关关系。
另一项研究中包括各种血液恶性病患者8名,克拉屈滨按0.12mg/kg的剂量作2小时的静滴。滴注完毕时的平均血浆浓度为48±19ng/ml。可用双相或三相消除模型解释克拉屈滨在其中5位患者体内的消除过程。肾功能正常患者的终末半衰期为5.4h,清除率为978±422ml/kg/h,稳态分布容积为4.5±2.8L/kg。本品可以透过血脑屏障,脑脊液中的浓度约为血浆浓度的25%。血浆蛋白结合率约为20%。
除已知的细胞毒作用机制外,目前尚不清楚本品在人体的代谢情况。实体瘤患者,按克拉屈滨3.5-8.1mg/m2/d的剂量连续静脉滴注5日,其尿排泄率平均为18%。目前尚未在肾功和肝功损伤患者体内进行克拉屈滨的消除研究。
【临床研究】
尚缺乏在中国人应用的临床研究资料。
国外已在需治疗的、处于毛细胞白血病活动期的患者体内进行了克拉屈滨注射液的2项开放单中心临床研究。89位病人参与Scripps临床教学和研究基地的研究(研究A),给药方案为静脉注射克拉屈滨注射液0.09mg/kg/d×7d。35位病人参与M.D.安德森癌症中心的研究(研究B),给药方案为静脉注射3.6mg/m2/d×7da的克拉屈滨注射液。完全反应(CR)的标准为:外周血和骨髓毛细胞被清除,血红蛋白恢复至12g/dl,血小板计数为100×109/L,绝对中性粒细胞计数为1500×106/L。好的部分反应(GPR)标准为:血液学参数与完全反应的一致,骨髓毛细胞剩余量小于5%。部分反应(PR)标准为:骨髓毛细胞至少降低50%,且血液学参数与完全反应一致。病理复发标准为:骨髓毛细胞增至治疗前的25%。临床复发标准为:血细胞减少复发,特别是,血红蛋白降低值≥2g/dl,绝对中性粒细胞计数(ANC)降低值≥25%或血小板计数降低值≥50000。如果发现符合完全反应标准的病人随后出现骨髓毛细胞(<治疗前的25%),我们将其归类为部分反应而不是完全反应的复发。
可评价有效性的患者(N=106),用上述血液学和骨髓反应标准评价其反应率,克拉屈滨注射液治疗后研究A和研究B的完全反应率分别为65%和68%,产生的联合完全反应率为66%。研究A和研究B的全部反应率(即完全反应+好的部分反应+部分反应)分别为89%和86%,联合全部反应率为88%。
使用ITT(intention-to-treat)分析,且CR标准需有无脾肿大的依据(即体检时无可触及脾和CT扫描≤13cm),研究A和研究B完全反应率分别为54%和53%,联合完全反应率为54%。研究A和研究B的全部反应率(CR+GPR+PR)分别为90%和85%,联合全部反应率为89%。
完全反应病人反应(即骨髓、外周血无毛细胞和外周血参数正常化)的中位时间(治疗开始时测量)大约为4个月。由于骨髓吸引术和活组织检查未经常在外周血正常化时进行,所以实际上完全反应的中数时间可能比记录的时间稍短。试验截止时完全反应的中数持续时间为8-25个月。93位反应病人在试验截止时有7位的疾病有所进展,4位无外周血异常(病理过程),仅局限于骨髓,3位病人出现外周血异常(临床过程)。7位对克拉屈滨注射液第一疗程无反应的病人接受了第二疗程的治疗。有足够随访、附加疗程的5位病人未改善其全部反应。
【适应症】本品可试用于经干扰素治疗失败后活动性的伴有临床意义的贫血、中性粒细胞减少、血少板减少以及疾病相关症状的毛细胞白血病(HCL)治疗。
【用法与用量】静脉滴注。治疗多毛细胞白血病时的建议剂量为克拉屈滨0.09mg/kg/d,作24小时的连续滴注,连用7天。不推荐其它的用药方案。根据己有经验,如患者对初始疗程无效,增加疗程不会获得更大利益。临用前按计算量。
【贮藏】2-8度冷藏。
---------------------------------------------------------------
原产地英文商品名:
LEUSTATIN 1mg/ml 10mls/vial
原产地英文药品名:
CLADRIBINE
中文参考商品译名:
LEUSTATIN 1毫克/毫升 10毫升/瓶
中文参考药品译名:
克拉屈滨
中文参考化合物名称:
2-氯-6-氨基-9-(2-脱氧-β-D-赤型-呋喃戊糖基)嘌呤
生产厂家中文参考译名:
ORTHO BIOTECH
生产厂家英文名:
ORTHO BIOTECH

---------------------------------------------------------------
原产地英文商品名:
CLADRIBINE(LEUSTATIN GENERIC)1mg/ml 10mls/vial
原产地英文药品名:
CLADRIBINE
中文参考商品译名:
克拉屈滨(LEUSTATIN仿制药)1毫克/毫升 10毫升/瓶
中文参考药品译名:
克拉屈滨
中文参考化合物名称:
2-氯-6-氨基-9-(2-脱氧-β-D-赤型-呋喃戊糖基)嘌呤
生产厂家中文参考译名:
APP
生产厂家英文名:
APP

---------------------------------------------------------------
Rx ONLY
For Intravenous Infusion Only
WARNINGS
Cladribine Injection should be administered under the supervision of a qualified physician experienced in the use of antineoplastic therapy. Suppression of bone marrow function should be anticipated. This is usually reversible and appears to be dose dependent. Serious neurological toxicity (including irreversible paraparesis and quadraparesis) has been reported in patients who received cladribine injection by continuous infusion at high doses (4 to 9 times the recommended dose for Hairy Cell Leukemia). Neurologic toxicity appears to demonstrate a dose relationship; however, severe neurological toxicity has been reported rarely following treatment with standard cladribine dosing regimens.
Acute nephrotoxicity has been observed with high doses of cladribine (4 to 9 times the recommended dose for Hairy Cell Leukemia), especially when given concomitantly with other nephrotoxic agents/therapies.
Cladribine Injection (also commonly known as 2-chloro-2´-deoxy-ß-D-adenosine) is a synthetic antineoplastic agent for continuous intravenous infusion. It is a clear, colorless, sterile, preservative-free, isotonic solution. Cladribine Injection is available in single-use vials containing 10 mg (1 mg/mL) of cladribine, a chlorinated purine nucleoside analog. Each mL of cladribine injection contains 1 mg of the active ingredient and 9 mg (0.15 mEq) of sodium chloride as an inactive ingredient. The solution has a pH range of 5.5 to 8.0. Phosphoric acid and/or dibasic sodium phosphate may have been added to adjust the pH to 6.3 ± 0.3.
The chemical name for cladribine is 2-chloro-6-amino-9-(2-deoxy-ß-D-erythro-pentofuranosyl)purine and the structure is represented below:
Molecular Formula = CHClNO Molecular Weight = 285.69
The selective toxicity of 2-chloro-2´-deoxy-ß-D-adenosine towards certain normal and malignant lymphocyte and monocyte populations is based on the relative activities of deoxycytidine kinase and deoxynucleotidase. Cladribine passively crosses the cell membrane. In cells with a high ratio of deoxycytidine kinase to deoxynucleotidase, it is phosphorylated by deoxycytidine kinase to 2-chloro-2´-deoxy-ß-D-adenosine monophosphate (2-CdAMP). Since 2-chloro-2´-deoxy-ß-D-adenosine is resistant to deamination by adenosine deaminase and there is little deoxynucleotide deaminase in lymphocytes and monocytes, 2-CdAMP accumulates intracellularly and is subsequently converted into the active triphosphate deoxynucleotide, 2-chloro-2´-deoxy-ß-D-adenosine triphosphate (2-CdATP). It is postulated that cells with high deoxycytidine kinase and low deoxynucleotidase activities will be selectively killed by 2-chloro-2´-deoxy-ß-D-adenosine as toxic deoxynucleotides accumulate intracellularly.
Cells containing high concentrations of deoxynucleotides are unable to properly repair single-strand DNA breaks. The broken ends of DNA activate the enzyme poly (ADP-ribose) polymerase resulting in NAD and ATP depletion and disruption of cellular metabolism. There is evidence, also, that 2-CdATP is incorporated into the DNA of dividing cells, resulting in impairment of DNA synthesis. Thus, 2-chloro-2´-deoxy-ß-D-adenosine can be distinguished from other chemotherapeutic agents affecting purine metabolism in that it is cytotoxic to both actively dividing and quiescent lymphocytes and monocytes, inhibiting both DNA synthesis and repair.
In a clinical investigation, 17 patients with Hairy Cell Leukemia and normal renal function were treated for 7 days with the recommended treatment regimen of cladribine (0.09 mg/kg/day) by continuous intravenous infusion. The mean steady-state serum concentration was estimated to be 5.7 ng/mL with an estimated systemic clearance of 663.5 mL/h/kg when cladribine was given by continuous infusion over 7 days. In Hairy Cell Leukemia patients, there does not appear to be a relationship between serum concentrations and ultimate clinical outcome.
In another study, 8 patients with hematologic malignancies received a two (2) hour infusion of cladribine (0.12 mg/kg). The mean end-of-infusion plasma cladribine concentration was 48 ± 19 ng/mL. For 5 of these patients, the disappearance of cladribine could be described by either a biphasic or triphasic decline. For these patients with normal renal function, the mean terminal half-life was 5.4 hours. Mean values for clearance and steady-state volume of distribution were 978 ± 422 mL/h/kg and 4.5 ± 2.8 L/kg, respectively.
Cladribine plasma concentration after intravenous administration declines multi-exponentially with an average half-life of 6.7 + 2.5 hours. In general, the apparent volume of distribution of cladribine is approximately 9 L/kg, indicating an extensive distribution in body tissues.
Cladribine penetrates into cerebrospinal fluid. One report indicates that concentrations are approximately 25% of those in plasma.
Cladribine is bound approximately 20% to plasma proteins.
Except for some understanding of the mechanism of cellular toxicity, no other information is available on the metabolism of cladribine in humans. An average of 18% of the administered dose has been reported to be excreted in urine of patients with solid tumors during a 5-day continuous intravenous infusion of 3.5 to 8.1 mg/m/day of cladribine. The effect of renal and hepatic impairment on the elimination of cladribine has not been investigated in humans.
Two single-center open label studies of cladribine have been conducted in patients with Hairy Cell Leukemia with evidence of active disease requiring therapy. In the study conducted at the Scripps Clinic and Research Foundation (Study A), 89 patients were treated with a single course of cladribine given by continuous intravenous infusion for 7 days at a dose of 0.09 mg/kg/day. In the study conducted at the M.D. Anderson Cancer Center (Study B), 35 patients were treated with a 7 day continuous intravenous infusion of cladribine at a comparable dose of 3.6 mg/m/day. A complete response (CR) required clearing of the peripheral blood and bone marrow of hairy cells and recovery of the hemoglobin to 12 g/dL, platelet count to 100 x 10/L, and absolute neutrophil count to 1500 x 10/L. A good partial response (GPR) required the same hematologic parameters as a complete response, and that fewer than 5% hairy cells remain in the bone marrow. A partial response (PR) required that hairy cells in the bone marrow be decreased by at least 50% from baseline and the same response for hematologic parameters as for complete response. A pathologic relapse was defined as an increase in bone marrow hairy cells to 25% of pretreatment levels. A clinical relapse was defined as the recurrence of cytopenias, specifically, decreases in hemoglobin ≥ 2 g/dL, ANC ≥ 25% or platelet counts ≥ 50,000. Patients who met the criteria for a complete response but subsequently were found to have evidence of bone marrow hairy cells (<25% of pretreatment levels) were reclassified as partial responses and were not considered to be complete responses with relapse.
Among patients evaluable for efficacy (N=106), using the hematologic and bone marrow response criteria described above, the complete response rates in patients treated with cladribine were 65% and 68% for Study A and Study B, respectively, yielding a combined complete response rate of 66%. Overall response rates (i.e., Complete plus Good Partial plus Partial Responses) were 89% and 86% in Study A and Study B, respectively, for a combined overall response rate of 88% in evaluable patients treated with cladribine.
Using an intent-to-treat analysis (N=123) and further requiring no evidence of splenomegaly as a criterion for CR (i.e., no palpable spleen on physical examination and ≤ 13 cm on CT scan), the complete response rates for Study A and Study B were 54% and 53%, respectively, giving a combined CR rate of 54%. The overall response rates (CR + GPR + PR) were 90% and 85%, for Studies A and B, respectively, yielding a combined overall response rate of 89%.
In these studies, 60% of the patients had not received prior chemotherapy for Hairy Cell Leukemia or had undergone splenectomy as the only prior treatment and were receiving cladribine as a first-line treatment. The remaining 40% of the patients received cladribine as a second-line treatment, having been treated previously with other agents, including α-interferon and/or deoxycoformycin. The overall response rate for patients without prior chemotherapy was 92%, compared with 84% for previously treated patients. Cladribine is active in previously treated patients; however, retrospective analysis suggests that the overall response rate is decreased in patients previously treated with splenectomy or deoxycoformycin and in patients refractory to α-interferon.
After a reversible decline, normalization of peripheral blood counts (Hemoglobin >12 g/dL, Platelets >100 x 10/L, Absolute Neutrophil Count (ANC) >1500 x 10/L) was achieved by 92% of evaluable patients. The median time to normalization of peripheral counts was 9 weeks from the start of treatment (Range: 2 to 72). The median time to normalization of Platelet Count was 2 weeks, the median time to normalization of ANC was 5 weeks and the median time to normalization of Hemoglobin was 8 weeks. With normalization of Platelet Count and Hemoglobin, requirements for platelet and RBC transfusions were abolished after Months 1 and 2, respectively, in those patients with complete response. Platelet recovery may be delayed in a minority of patients with severe baseline thrombocytopenia. Corresponding to normalization of ANC, a trend toward a reduced incidence of infection was seen after the third month, when compared to the months immediately preceding cladribine therapy (see also WARNINGS, PRECAUTIONS and ADVERSE REACTIONS).
For patients achieving a complete response, the median time to response (i.e., absence of hairy cells in bone marrow and peripheral blood together with normalization of peripheral blood parameters), measured from treatment start, was approximately 4 months. Since bone marrow aspiration and biopsy were frequently not performed at the time of peripheral blood normalization, the median time to complete response may actually be shorter than that which was recorded. At the time of data cut- off, the median duration of complete response was greater than 8 months and ranged to 25+ months. Among 93 responding patients, seven had shown evidence of disease progression at the time of the data cut-off. In four of these patients, disease was limited to the bone marrow without peripheral blood abnormalities (pathologic progression), while in three patients there were also peripheral blood abnormalities (clinical progression). Seven patients who did not respond to a first course of cladribine received a second course of therapy. In the five patients who had adequate follow-up, additional courses did not appear to improve their overall response.
| RESPONSE RATES TO CLADRIBINE TREATMENT IN PATIENTS WITH HAIRY CELL LEUKEMIA |
|
| CR |
Overall |
| Evaluable PatientsN=106 |
66% |
88% |
| Intent-to-treat PopulationN=123 |
54% |
89% |
| OVERALL RESPONSE RATES (CR + GPR + PR) TO CLADRIBINE TREATMENT IN PATIENTS WITH HAIRY CELL LEUKEMIA |
|
| OVERALL RESPONSE(N=123) |
NRNR = No Response + RELAPSE |
| No Prior Chemotherapy |
68/74
92% |
6 + 4
14% |
| Any Prior Chemotherapy |
41/49
84% |
8 + 3
22% |
| Previous Splenectomy |
32/41P<0.05
78% |
9 + 1
24% |
| Previous Interferon |
40/48
83% |
8 + 3
23% |
| Interferon Refractory |
6/11
55% |
5 + 2
64% |
| Previous Deoxycoformycin |
3/6
50% |
3 + 1
66% |
| CLADRIBINE TREATMENT IN PATIENTS WITH HAIRY CELL LEUKEMIA TIME TO NORMALIZATION OF PERIPHERAL BLOOD COUNTS |
| Parameter |
Median Time to Normalization of CountDay 1 = First day of infusion |
| Platelet Count |
2 weeks |
| Absolute Neutrophil Count |
5 weeks |
| Hemoglobin |
8 weeks |
| ANC, Hemoglobin and Platelet Count |
9 weeks |
Cladribine is indicated for the treatment of active Hairy Cell Leukemia as defined by clinically significant anemia, neutropenia, thrombocytopenia or disease-related symptoms.
Cladribine is contraindicated in those patients who are hypersensitive to this drug or any of its components.
Severe bone marrow suppression, including neutropenia, anemia and thrombocytopenia, has been commonly observed in patients treated with cladribine, especially at high doses. At initiation of treatment, most patients in the clinical studies had hematologic impairment as a manifestation of active Hairy Cell Leukemia. Following treatment with cladribine, further hematologic impairment occurred before recovery of peripheral blood counts began. During the first two weeks after treatment initiation, mean Platelet Count, ANC, and Hemoglobin concentration declined and subsequently increased with normalization of mean counts by Day 12, Week 5 and Week 8, respectively. The myelosuppressive effects of cladribine were most notable during the first month following treatment. Forty-four percent (44%) of patients received transfusions with RBCs and 14% received transfusions with platelets during Month 1. Careful hematologic monitoring, especially during the first 4 to 8 weeks after treatment with cladribine, is recommended (see PRECAUTIONS).
Fever (T ≥ 100˚ F) was associated with the use of cladribine in approximately two-thirds of patients (131/196) in the first month of therapy. Virtually all of these patients were treated empirically with parenteral antibiotics. Overall, 47% (93/196) of all patients had fever in the setting of neutropenia (ANC ≤ 1000), including 62 patients (32%) with severe neutropenia (i.e., ANC ≤ 500).
In a Phase I investigational study using cladribine in high doses (4 to 9 times the recommended dose for Hairy Cell Leukemia) as part of a bone marrow transplant conditioning regimen, which also included high dose cyclophosphamide and total body irradiation, acute nephrotoxicity and delayed onset neurotoxicity were observed. Thirty-one (31) poor-risk patients with drug-resistant acute leukemia in relapse (29 cases) or non-Hodgkins Lymphoma (2 cases) received cladribine for 7 to 14 days prior to bone marrow transplantation. During infusion, 8 patients experienced gastrointestinal symptoms. While the bone marrow was initially cleared of all hematopoietic elements, including tumor cells, leukemia eventually recurred in all treated patients. Within 7 to 13 days after starting treatment with cladribine, 6 patients (19%) developed manifestations of renal dysfunction (e.g., acidosis, anuria, elevated serum creatinine, etc.) and 5 required dialysis. Several of these patients were also being treated with other medications having known nephrotoxic potential. Renal dysfunction was reversible in 2 of these patients. In the 4 patients whose renal function had not recovered at the time of death, autopsies were performed; in 2 of these, evidence of tubular damage was noted. Eleven (11) patients (35%) experienced delayed onset neurologic toxicity. In the majority, this was characterized by progressive irreversible motor weakness (paraparesis/quadriparesis), of the upper and/or lower extremities, first noted 35 to 84 days after starting high dose therapy with cladribine. Non-invasive testing (electromyography and nerve conduction studies) was consistent with demyelinating disease. Severe neurologic toxicity has also been noted with high doses of another drug in this class.
Axonal peripheral polyneurophathy was observed in a dose escalation study at the highest dose levels (approximately 4 times the recommended dose for Hairy Cell Leukemia) in patients not receiving cyclophosphamide or total body irradiation. Severe neurological toxicity has been reported rarely following treatment with standard cladribine dosing regimens.
In patients with Hairy Cell Leukemia treated with the recommended treatment regimen (0.09 mg/kg/day for 7 consecutive days), there have been no reports of nephrologic toxicities.
Of the 196 Hairy Cell Leukemia patients entered in the two trials, there were 8 deaths following treatment. Of these, 6 were of infectious etiology, including 3 pneumonias, and 2 occurred in the first month following cladribine therapy. Of the 8 deaths, 6 occurred in previously treated patients who were Refractory to α-interferon.
Benzyl alcohol is a constituent of the recommended diluent for the 7-day infusion solution. Benzyl alcohol has been reported to be associated with a fatal “Gasping Syndrome” in premature infants (see DOSAGE AND ADMINISTRATION).
Cladribine should not be given during pregnancy.
Cladribine is teratogenic in mice and rabbits and consequently has the potential to cause fetal harm when administered to a pregnant woman. A significant increase in fetal variations was observed in mice receiving 1.5 mg/kg/day (4.5 mg/m) and increased resorptions, reduced litter size and increased fetal malformations were observed when mice received 3 mg/kg/day (9 mg/m). Fetal death and malformations were observed in rabbits that received 3 mg/kg/day (33 mg/m). No fetal effects were seen in mice at 0.5 mg/kg/day (1.5 mg/m) or in rabbits at 1 mg/kg/day (11 mg/m).
Although there is no evidence of teratogenicity in humans due to cladribine, other drugs which inhibit DNA synthesis (e.g., methotrexate and aminopterin) have been reported to be teratogenic in humans. Cladribine has been shown to be embryotoxic in mice when given at doses equivalent to the recommended dose.
There are no adequate and well controlled studies in pregnant women. If cladribine is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing age should be advised to avoid becoming pregnant.
Cladribine is a potent antineoplastic agent with potentially significant toxic side effects. It should be administered only under the supervision of a physician experienced with the use of cancer chemotherapeutic agents. Patients undergoing therapy should be closely observed for signs of hematologic and non-hematologic toxicity. Periodic assessment of peripheral blood counts, particularly during the first 4 to 8 weeks post-treatment, is recommended to detect the development of anemia, neutropenia and thrombocytopenia and for early detection of any potential sequelae (e.g., infection or bleeding). As with other potent chemotherapeutic agents, monitoring of renal and hepatic function is also recommended, especially in patients with underlying kidney or liver dysfunction (see WARNINGS and ADVERSE REACTIONS).
Fever was a frequently observed side effect during the first month on study. Since the majority of fevers occurred in neutropenic patients, patients should be closely monitored during the first month of treatment and empiric antibiotics should be initiated as clinically indicated. Although 69% of patients developed fevers, less than 1/3 of febrile events were associated with documented infection.
Given the known myelosuppressive effects of cladribine, practitioners should carefully evaluate the risks and benefits of administering this drug to patients with active infections (see WARNINGS and ADVERSE REACTIONS).
There are inadequate data on dosing of patients with renal or hepatic insufficiency. Development of acute renal insufficiency in some patients receiving high doses of cladribine has been described. Until more information is available, caution is advised when administering the drug to patients with known or suspected renal or hepatic insufficiency (see WARNINGS).
Rare cases of tumor lysis syndrome have been reported in patients treated with cladribine with other hematologic malignancies having a high tumor burden.
Cladribine must be diluted in designated intravenous solutions prior to administration (see DOSAGE AND ADMINISTRATION).
During and following treatment, the patient’s hematologic profile should be monitored regularly to determine the degree of hematopoietic suppression. In the clinical studies, following reversible declines in all cell counts, the mean Platelet Count reached 100 x 10/L by Day 12, the mean Absolute Neutrophil Count reached 1500 x 10/L by Week 5 and the mean Hemoglobin reached 12 g/dL by Week 8. After peripheral counts have normalized, bone marrow aspiration and biopsy should be performed to confirm response to treatment with cladribine. Febrile events should be investigated with appropriate laboratory and radiologic studies. Periodic assessment of renal function and hepatic function should be performed as clinically indicated.
There are no known drug interactions with cladribine. Caution should be exercised if cladribine is administered before, after, or in conjunction with other drugs known to cause immunosuppression or myelosuppression (see WARNINGS).
No animal carcinogenicity studies have been conducted with cladribine. However, its carcinogenic potential cannot be excluded based on demonstrated genotoxicity of cladribine.
As expected for compounds in this class, the actions of cladribine yield DNA damage. In mammalian cells in culture, cladribine caused the accumulation of DNA strand breaks. Cladribine was also incorporated into DNA of human lymphoblastic leukemia cells. Cladribine was not mutagenic in vitro (Ames and Chinese hamster ovary cell gene mutation tests) and did not induce unscheduled DNA synthesis in primary rat hepatocyte cultures. However, cladribine was clastogenic both in vitro (chromosome aberrations in Chinese hamster ovary cells) and in vivo (mouse bone marrow micronucleus test).
When administered intravenously to Cynomolgus monkeys, cladribine has been shown to cause suppression of rapidly generating cells, including testicular cells. The effect on human fertility is unknown.
See WARNINGS.
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from cladribine, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug for the mother.
Safety and effectiveness in pediatric patients have not been established. In a Phase I study involving patients 1 to 21 years old with relapsed acute leukemia, cladribine was given by continuous intravenous infusion in doses ranging from 3 to 10.7 mg/m/day for 5 days (one-half to twice the dose recommended in Hairy Cell Leukemia). In this study, the dose-limiting toxicity was severe myelosuppression with profound neutropenia and thrombocytopenia. At the highest dose (10.7 mg/m/day), 3 of 7 patients developed irreversible myelosuppression and fatal systemic bacterial or fungal infections. No unique toxicities were noted in this study (see WARNINGS and ADVERSE REACTIONS).
Clinical studies of cladribine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy in elderly patients.
Safety data are based on 196 patients with Hairy Cell Leukemia: the original cohort of 124 patients plus an additional 72 patients enrolled at the same two centers after the original enrollment cutoff. In Month 1 of the Hairy Cell Leukemia clinical trials, severe neutropenia was noted in 70% of patients, fever in 69%, and infection was documented in 28%. Other adverse experiences reported frequently during the first 14 days after initiating treatment included: fatigue (45%), nausea (28%), rash (27%), headache (22%) and injection site reactions (19%). Most non-hematologic adverse experiences were mild to moderate in severity.
Myelosuppression was frequently observed during the first month after starting treatment. Neutropenia (ANC < 500 x 10/L) was noted in 70% of patients, compared with 26% in whom it was present initially. Severe anemia (Hemoglobin <8.5 g/dL) developed in 37% of patients, compared with 10% initially and thrombocytopenia (Platelets < 20 x 10/L) developed in 12% of patients, compared to 4% in whom it was noted initially.
During the first month, 54 of 196 patients (28%) exhibited documented evidence of infection. Serious infections (e.g., septicemia, pneumonia) were reported in 6% of all patients; the remainder were mild or moderate. Several deaths were attributable to infection and/or complications related to the underlying disease. During the second month, the overall rate of documented infection was 6%; these infections were mild to moderate and no severe systemic infections were seen. After the third month, the monthly incidence of infection was either less than or equal to that of the months immediately preceding cladribine therapy.
During the first month, 11% of patients experienced severe fever (i.e., ≥104°F). Documented infections were noted in fewer than one-third of febrile episodes. Of the 196 patients studied, 19 were noted to have a documented infection in the month prior to treatment. In the month following treatment, there were 54 episodes of documented infection: 23 (42%) were bacterial, 11 (20%) were viral and 11 (20%) were fungal. Seven (7) of 8 documented episodes of herpes zoster occurred during the month following treatment. Fourteen (14) of 16 episodes of documented fungal infections occurred in the first two months following treatment. Virtually all of these patients were treated empirically with antibiotics (see WARNINGS and PRECAUTIONS).
Analysis of lymphocyte subsets indicates that treatment with cladribine is associated with prolonged depression of the CD4 counts. Prior to treatment, the mean CD4 count was 766/µL. The mean CD4 count nadir, which occurred 4 to 6 months following treatment, was 272/µL. Fifteen (15) months after treatment, mean CD4 counts remained below 500/µL. CD8 counts behaved similarly, though increasing counts were observed after 9 months. The clinical significance of the prolonged CD4 lymphopenia is unclear.
Another event of unknown clinical significance includes the observation of prolonged bone marrow hypocellularity. Bone marrow cellularity of <35% was noted after 4 months in 42 of 124 patients (34%) treated in the two pivotal trials. This hypocellularity was noted as late as day 1010. It is not known whether the hypocellularity is the result of disease related marrow fibrosis or if it is the result of cladribine toxicity. There was no apparent clinical effect on the peripheral blood counts.
The vast majority of rashes were mild and occurred in patients who were receiving or had recently been treated with other medications (e.g., allopurinol or antibiotics) known to cause rash.
Most episodes of nausea were mild, not accompanied by vomiting, and did not require treatment with antiemetics. In patients requiring antiemetics, nausea was easily controlled, most frequently with chlorpromazine.
Adverse reactions reported during the first 2 weeks following treatment initiation (regardless of relationship to drug) by >5% of patients included:
Body as a Whole : fever (69%), fatigue (45%), chills (9%), asthenia (9%), diaphoresis (9%), malaise (7%), trunk pain (6%)
Gastrointestinal : nausea (28%), decreased appetite (17%), vomiting (13%), diarrhea (10%), constipation (9%), abdominal pain (6%)
Hemic/Lymphatic: purpura (10%), petechiae (8%), epistaxis (5%)
Nervous System: headache (22%), dizziness (9%), insomnia (7%)
Cardiovascular System: edema (6%), tachycardia (6%)
Respiratory System: abnormal breath sounds (11%), cough (10%), abnormal chest sounds (9%), shortness of breath (7%)
Skin/Subcutaneous Tissue: rash (27%), injection site reactions (19%), pruritis (6%), pain (6%), erythema (6%)
Musculoskeletal System: myalgia (7%), arthralgia (5%)
Adverse experiences related to intravenous administration included: injection site reactions (9%) (i.e., redness, swelling, pain), thrombosis (2%), phlebitis (2%) and a broken catheter (1%).
These appear to be related to the infusion procedure and/or indwelling catheter, rather than the medication or the vehicle. From Day 15 to the last follow-up visit, the only events reported by >5% of patients were: fatigue (11%), rash (10%), headache (7%), cough (7%), and malaise (5%).
For a description of adverse reactions associated with use of high doses in non-Hairy Cell Leukemia patients, see WARNINGS.
The following additional adverse events have been reported since the drug became commercially available. These adverse events have been reported primarily in patients who received multiple courses of cladribine:
Hematologic: bone marrow suppression with prolonged pancytopenia, including some reports of aplastic anemia; hemolytic anemia, which was reported in patients with lymphoid malignancies, occurring within the first few weeks following treatment. Rare cases of myelodysplastic syndrome have been reported.
Hepatic: reversible, generally mild increases in bilirubin and transaminases.
Nervous System: Neurological toxicity; however, severe neurotoxicity has been reported rarely following treatment with standard cladribine dosing regimens.
Respiratory System: pulmonary interstitial infiltrates; in most cases, an infectious etiology was identified.
Skin/Subcutaneous: urticaria, hypereosinophilia. In isolated cases Stevens-Johnson and toxic epidermal necrolysis have been reported in patients who were receiving or had recently been treated with other medications (e.g., allopurinol or antibiotics) known to cause these syndromes.
Opportunistic infections have occurred in the acute phase of treatment due to the immunosuppression mediated by cladribine.
High doses of cladribine have been associated with: irreversible neurologic toxicity (paraparesis/quadriparesis), acute nephrotoxicity, and severe bone marrow suppression resulting in neutropenia, anemia and thrombocytopenia (see WARNINGS). There is no known specific antidote to overdosage. Treatment of overdosage consists of discontinuation of cladribine, careful observation and appropriate supportive measures. It is not known whether the drug can be removed from the circulation by dialysis or hemofiltration.
The recommended dose and schedule of cladribine for active Hairy Cell Leukemia is as a single course given by continuous infusion for 7 consecutive days at a dose of 0.09 mg/kg/day. Deviations from this dosage regimen are not advised. If the patient does not respond to the initial course of cladribine for Hairy Cell Leukemia, it is unlikely that they will benefit from additional courses. Physicians should consider delaying or discontinuing the drug if neurotoxicity or renal toxicity occurs (see WARNINGS).
Specific risk factors predisposing to increased toxicity from cladribine have not been defined. In view of the known toxicities of agents of this class, it would be prudent to proceed carefully in patients with known or suspected renal insufficiency or severe bone marrow impairment of any etiology. Patients should be monitored closely for hematologic and non-hematologic toxicity (see WARNINGS and PRECAUTIONS).
Cladribine must be diluted with the designated diluent prior to administration. Since the drug product does not contain any antimicrobial preservative or bacteriostatic agent, aseptic technique and proper environmental precautions must be observed in preparation of cladribine solutions.
Add the calculated dose (0.09 mg/kg or 0.09 mL/kg) of cladribine to an infusion bag containing 500 mL of 0.9% Sodium Chloride Injection. Infuse continuously over 24 hours. Repeat daily for a total of 7 consecutive days. The use of 5% dextrose as a diluent is not recommended because of increased degradation of cladribine. Admixtures of cladribine are chemically and physically stable for at least 24 hours at room temperature under normal room fluorescent light in Baxter Viaflex®† PVC infusion containers. Since limited compatibility data are available, adherence to the recommended diluents and infusion systems is advised.
|
| Dose of
Cladribine Injection |
Recommended Diluent |
Quantity of Diluent |
24 hour
infusion method |
1 (day) x 0.09 mg/kg |
0.9% Sodium Chloride Injection |
500 mL |
The 7 day infusion solution should only be prepared with Bacteriostatic 0.9% Sodium Chloride Injection (0.9% benzyl alcohol preserved). In order to minimize the risk of microbial contamination, both cladribine injection and the diluent should be passed through a sterile 0.22µ disposable hydrophilic syringe filter as each solution is being introduced into the infusion reservoir. First add the calculated dose of cladribine (7 days x 0.09 mg/kg or mL/kg) to the infusion reservoir through the sterile filter.
Then add a calculated amount of Bacteriostatic 0.9% Sodium Chloride Injection (0.9% benzyl alcohol preserved) also through the filter to bring the total volume of the solution to 100 mL. After completing solution preparation, clamp off the line, disconnect and discard the filter. Aseptically aspirate air bubbles from the reservoir as necessary using the syringe and a dry second sterile filter or a sterile vent filter assembly. Reclamp the line and discard the syringe and filter assembly. Infuse continuously over 7 days. Solutions prepared with Bacteriostatic Sodium Chloride Injection for individuals weighing more than 85 kg may have reduced preservative effectiveness due to greater dilution of the benzyl alcohol preservative. Admixtures for the 7 day infusion have demonstrated acceptable chemical and physical stability for at least 7 days in the SIMS Deltec MEDICATION CASSETTE™ Reservoir .
Since limited compatibility data are available, adherence to the recommended diluents and infusion systems is advised. Solutions containing cladribine should not be mixed with other intravenous drugs or additives or infused simultaneously via a common intravenous line, since compatibility testing has not been performed. Preparations containing benzyl alcohol should not be used in neonates (see WARNINGS).
Care must be taken to assure the sterility of prepared solutions. Once diluted, solutions of cladribine should be administered promptly or stored in the refrigerator (2° to 8° C) for no more than 8 hours prior to start of administration. Vials of cladribine are for single-use only. Any unused portion should be discarded in an appropriate manner (see Handling and Disposal ).
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. A precipitate may occur during the exposure of cladribine to low temperatures; it may be resolubilized by allowing the solution to warm naturally to room temperature and by shaking vigorously. DO NOT HEAT OR MICROWAVE.
|
| Dose ofCladribine Injection |
Recommended Diluent |
Quantity of Diluent |
| 7 day infusion method(use sterile 0.22µ filter when preparing infusion solution) |
7 (days) x 0.09 mg/kg |
Bacteriostatic 0.9% Sodium Chloride Injection (0.9% benzyl alcohol) |
q.s. to 100 mL |
When stored in refrigerated conditions between 2° to 8° C (36° to 46° F) protected from light, unopened vials of cladribine are stable until the expiration date indicated on the package. Freezing does not adversely affect the solution. If freezing occurs, thaw naturally to room temperature. DO NOT heat or microwave. Once thawed, the vial of cladribine is stable until expiry if refrigerated. DO NOT refreeze. Once diluted, solutions containing cladribine should be administered promptly or stored in the refrigerator (2° to 8° C) for no more than 8 hours prior to administration.
The potential hazards associated with cytotoxic agents are well established and proper precautions should be taken when handling, preparing, and administering cladribine. The use of disposable gloves and protective garments is recommended. If cladribine contacts the skin or mucous membranes, wash the involved surface immediately with copious amounts of water. Several guidelines on this subject have been published. There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate. Refer to your institution’s guidelines and all applicable state/local regulations for disposal of cytotoxic waste.
Cladribine Injection is supplied as a sterile, preservative-free, isotonic solution containing 10 mg (1 mg/mL) of cladribine as 10 mL filled into a single-use clear flint glass 20 mL vial, individually boxed. NDC 55390-115-01
Store refrigerated 2° to 8° C (36° to 46° F). Protect from light during storage.
†Viaflex containers, manufactured by Baxter Healthcare Corporation - Code No. 2B8013 (tested in 1991)
MEDICATION CASSETTE™ Reservoir, manufactured by SIMS Deltec, Inc. - Reorder No. 602100A (tested in 1991)
Manufactured by: Distributed by:
Ben Venue Laboratories, Inc. Bedford Laboratories™
Bedford, OH 44146 Bedford, OH 44146
August 2006 CLD-P02
Novation, the supply company of VHA and UHC, and NOVAPLUS are trademarks of Novation, LLC. |