|
KEYTRUDA(pembrolizumab) injection, powder, lyophilized, for solution
1 INDICATIONS AND USAGE KEYTRUDA® (pembrolizumab) is indicated for the treatment of patients with unresectable or metastatic melanoma and disease progression following ipilimumab and, if BRAF V600 mutation positive, a BRAF inhibitor [see Clinical Studies (14)]. This indication is approved under accelerated approval based on tumor response rate and durability of response. An improvement in survival or disease-related symptoms has not yet been established. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trials. 2 DOSAGE AND ADMINISTRATION 2.1 Recommended Dosing The recommended dose of KEYTRUDA is 2 mg/kg administered as an intravenous infusion over 30 minutes every 3 weeks until disease progression or unacceptable toxicity. 2.2 Dose Modifications Withhold KEYTRUDA for any of the following:
Resume KEYTRUDA in patients whose adverse reactions recover to Grade 0-1. Permanently discontinue KEYTRUDA for any of the following:
2.3 Preparation and Administration Preparation
Storage of Reconstituted and Diluted Solutions The product does not contain a preservative. Store the reconstituted and diluted solutions of KEYTRUDA either:
Do not freeze. Administration
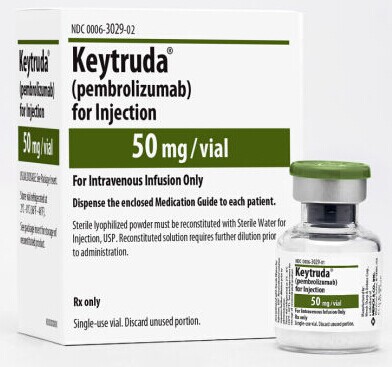
3 DOSAGE FORMS AND STRENGTHS For injection: 50 mg lyophilized powder in a single-use vial for reconstitution 4 CONTRAINDICATIONS None. 5 WARNINGS AND PRECAUTIONS 5.1 Immune-Mediated Pneumonitis Pneumonitis occurred in 12 (2.9%) of 411 melanoma patients, including Grade 2 or 3 cases in 8 (1.9%) and 1 (0.2%) patients, respectively, receiving KEYTRUDA in Trial 1. The median time to development of pneumonitis was 5 months (range 0.3 weeks-9.9 months). The median duration was 4.9 months (range 1 week-14.4 months). Five of eight patients with Grade 2 and the one patient with Grade 3 pneumonitis required initial treatment with high-dose systemic corticosteroids (greater than or equal to 40 mg prednisone or equivalent per day) followed by a corticosteroid taper. The median initial dose of high-dose corticosteroid treatment was 63.4 mg/day of prednisone or equivalent with a median duration of treatment of 3 days (range 1-34) followed by a corticosteroid taper. Pneumonitis led to discontinuation of KEYTRUDA in 3 (0.7%) patients. Pneumonitis completely resolved in seven of the nine patients with Grade 2-3 pneumonitis. Monitor patients for signs and symptoms of pneumonitis. Evaluate patients with suspected pneumonitis with radiographic imaging and administer corticosteroids for Grade 2 or greater pneumonitis. Withhold KEYTRUDA for moderate (Grade 2) pneumonitis, and permanently discontinue KEYTRUDA for severe (Grade 3) or life-threatening (Grade 4) pneumonitis [see Dosage and Administration (2.2) and Adverse Reactions (6.1)]. 5.2 Immune-Mediated Colitis Colitis (including microscopic colitis) occurred in 4 (1%) of 411 patients, including Grade 2 or 3 cases in 1 (0.2%) and 2 (0.5%) patients, respectively, receiving KEYTRUDA in Trial 1. The median time to onset of colitis was 6.5 months (range 2.3-9.8). The median duration was 2.6 months (range 0.6 weeks-3.6 months). All three patients with Grade 2 or 3 colitis were treated with high-dose corticosteroids (greater than or equal to 40 mg prednisone or equivalent per day) with a median initial dose of 70 mg/day of prednisone or equivalent; the median duration of initial treatment was 7 days (range 4-41), followed by a corticosteroid taper. One patient (0.2%) required permanent discontinuation of KEYTRUDA due to colitis. All four patients with colitis experienced complete resolution of the event. Monitor patients for signs and symptoms of colitis. Administer corticosteroids for Grade 2 or greater colitis. Withhold KEYTRUDA for moderate (Grade 2) or severe (Grade 3) colitis, and permanently discontinue KEYTRUDA for life-threatening (Grade 4) colitis [see Dosage and Administration (2.2) and Adverse Reactions (6.1)]. 5.3 Immune-Mediated Hepatitis Hepatitis (including autoimmune hepatitis) occurred in 2 (0.5%) of 411 patients, including a Grade 4 case in 1 (0.2%) patient, receiving KEYTRUDA in Trial 1. The time to onset was 22 days for the case of Grade 4 hepatitis which lasted 1.1 months. The patient with Grade 4 hepatitis permanently discontinued KEYTRUDA and was treated with high-dose (greater than or equal to 40 mg prednisone or equivalent per day) systemic corticosteroids followed by a corticosteroid taper. Both patients with hepatitis experienced complete resolution of the event. Monitor patients for changes in liver function. Administer corticosteroids for Grade 2 or greater hepatitis and, based on severity of liver enzyme elevations, withhold or discontinue KEYTRUDA [see Dosage and Administration (2.2) and Adverse Reactions (6.1)]. 5.4 Immune-Mediated Hypophysitis Hypophysitis occurred in 2 (0.5%) of 411 patients, consisting of one Grade 2 and one Grade 4 case (0.2% each), in patients receiving KEYTRUDA in Trial 1. The time to onset was 1.7 months for the patient with Grade 4 hypophysitis and 1.3 months for the patient with Grade 2 hypophysitis. Both patients were treated with high-dose (greater than or equal to 40 mg prednisone or equivalent per day) corticosteroids followed by a corticosteroid taper and remained on a physiologic replacement dose. Monitor for signs and symptoms of hypophysitis. Administer corticosteroids for Grade 2 or greater hypophysitis. Withhold KEYTRUDA for moderate (Grade 2) hypophysitis, withhold or discontinue KEYTRUDA for severe (Grade 3) hypophysitis, and permanently discontinue KEYTRUDA for life-threatening (Grade 4) hypophysitis [see Dosage and Administration (2.2) and Adverse Reactions (6.1)]. 5.5 Renal Failure and Immune-Mediated Nephritis Nephritis occurred in 3 (0.7%) patients, consisting of one case of Grade 2 autoimmune nephritis (0.2%) and two cases of interstitial nephritis with renal failure (0.5%), one Grade 3 and one Grade 4. The time to onset of autoimmune nephritis was 11.6 months after the first dose of KEYTRUDA (5 months after the last dose) and lasted 3.2 months; this patient did not have a biopsy. Acute interstitial nephritis was confirmed by renal biopsy in two patients with Grades 3-4 renal failure. All three patients fully recovered renal function with treatment with high-dose corticosteroids (greater than or equal to 40 mg prednisone or equivalent per day) followed by a corticosteroid taper. Monitor patients for changes in renal function. Administer corticosteroids for Grade 2 or greater nephritis. Withhold KEYTRUDA for moderate (Grade 2) nephritis, and permanently discontinue KEYTRUDA for severe (Grade 3), or life-threatening (Grade 4) nephritis [see Dosage and Administration (2.2) and Adverse Reactions (6.1)]. 5.6 Immune-Mediated Hyperthyroidism and Hypothyroidism Hyperthyroidism occurred in 5 (1.2%) of 411 patients, including Grade 2 or 3 cases in 2 (0.5%) and 1 (0.2%) patients, respectively, receiving KEYTRUDA in Trial 1. The median time to onset was 1.5 months (range 0.5-2.1). The median duration was 2.8 months (range 0.9 to 6.1). One of two patients with Grade 2 and the one patient with Grade 3 hyperthyroidism required initial treatment with high-dose corticosteroids (greater than or equal to 40 mg prednisone or equivalent per day) followed by a corticosteroid taper. One patient (0.2%) required permanent discontinuation of KEYTRUDA due to hyperthyroidism. All five patients with hyperthyroidism experienced complete resolution of the event. Hypothyroidism occurred in 34 (8.3%) of 411 patients, including a Grade 3 case in 1 (0.2%) patient, receiving KEYTRUDA in Trial 1. The median time to onset of hypothyroidism was 3.5 months (range 0.7 weeks-19 months). All but two of the patients with hypothyroidism were treated with long-term thyroid hormone replacement therapy. The other two patients only required short-term thyroid hormone replacement therapy. No patient received corticosteroids or discontinued KEYTRUDA for management of hypothyroidism. Thyroid disorders can occur at any time during treatment. Monitor patients for changes in thyroid function (at the start of treatment, periodically during treatment, and as indicated based on clinical evaluation) and for clinical signs and symptoms of thyroid disorders. Administer corticosteroids for Grade 3 or greater hyperthyroidism, withhold KEYTRUDA for severe (Grade 3) hyperthyroidism, and permanently discontinue KEYTRUDA for life-threatening (Grade 4) hyperthyroidism. Isolated hypothyroidism may be managed with replacement therapy without treatment interruption and without corticosteroids [see Dosage and Administration (2.2) and Adverse Reactions (6.1)]. 5.7 Other Immune-Mediated Adverse Reactions Other clinically important immune-mediated adverse reactions can occur. The following clinically significant, immune-mediated adverse reactions occurred in less than 1% of patients treated with KEYTRUDA in Trial 1: exfoliative dermatitis, uveitis, arthritis, myositis, pancreatitis, hemolytic anemia, partial seizures arising in a patient with inflammatory foci in brain parenchyma, and adrenal insufficiency. Across clinical studies with KEYTRUDA in approximately 2000 patients, the following additional clinically significant, immune-mediated adverse reactions were reported in less than 1% of patients: myasthenic syndrome, optic neuritis, and rhabdomyolysis. For suspected immune-mediated adverse reactions, ensure adequate evaluation to confirm etiology or exclude other causes. Based on the severity of the adverse reaction, withhold KEYTRUDA and administer corticosteroids. Upon improvement to Grade 1 or less, initiate corticosteroid taper and continue to taper over at least 1 month. Restart KEYTRUDA if the adverse reaction remains at Grade 1 or less. Permanently discontinue KEYTRUDA for any severe or Grade 3 immune-mediated adverse reaction that recurs and for any life-threatening immune-mediated adverse reaction [see Dosage and Administration (2.2) and Adverse Reactions (6.1)]. 5.8 Embryofetal Toxicity Based on its mechanism of action, KEYTRUDA may cause fetal harm when administered to a pregnant woman. Animal models link the PD-1/PDL-1 signaling pathway with maintenance of pregnancy through induction of maternal immune tolerance to fetal tissue. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus. Advise females of reproductive potential to use highly effective contraception during treatment with KEYTRUDA and for 4 months after the last dose of KEYTRUDA [see Use in Specific Populations (8.1, 8.8)]. 6 ADVERSE REACTIONS The following adverse reactions are discussed in greater detail in other sections of the labeling.
6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The data described in the WARNINGS and PRECAUTIONS section reflect exposure to KEYTRUDA in Trial 1, an uncontrolled, open-label, multiple cohort trial in which 411 patients with unresectable or metastatic melanoma received KEYTRUDA at either 2 mg/kg every 3 weeks or 10 mg/kg every 2 or 3 weeks. The median duration of exposure to KEYTRUDA was 6.2 months (range 1 day to 24.6 months) with a median of 10 doses (range 1 to 51). The study population characteristics were: median age of 61 years (range 18-94), 39% age 65 years or older, 60% male, 97% white, 73% with M1c disease, 8% with brain metastases, 35% with elevated LDH, 54% with prior exposure to ipilimumab, and 47% with two or more prior systemic therapies for advanced or metastatic disease. KEYTRUDA was discontinued for adverse reactions in 9% of the 411 patients. Adverse reactions, reported in at least two patients, that led to discontinuation of KEYTRUDA were: pneumonitis, renal failure, and pain. Serious adverse reactions occurred in 36% of patients receiving KEYTRUDA. The most frequent serious adverse drug reactions reported in 2% or more of patients in Trial 1 were renal failure, dyspnea, pneumonia, and cellulitis. Table 1 presents adverse reactions identified from analyses of the 89 patients with unresectable or metastatic melanoma who received KEYTRUDA 2 mg/kg every three weeks in one cohort of Trial 1. Patients had documented disease progression following treatment with ipilimumab and, if BRAF V600 mutation positive, a BRAF inhibitor. This cohort of Trial 1 excluded patients with severe immune-related toxicity related to ipilimumab, defined as any Grade 4 toxicity requiring treatment with corticosteroids or Grade 3 toxicity requiring corticosteroid treatment (greater than 10 mg/day prednisone or equivalent dose) for greater than 12 weeks; a medical condition that required systemic corticosteroids or other immunosuppressive medication; a history of pneumonitis or interstitial lung disease; or any active infection requiring therapy, including HIV or hepatitis B or C. Of the 89 patients in this cohort, the median age was 59 years (range 18-88), 33% were age 65 years or older, 53% were male, 98% were white, 44% had an elevated LDH, 84% had Stage M1c disease, 8% had brain metastases, and 70% received two or more prior therapies for advanced or metastatic disease. The median duration of exposure to KEYTRUDA was 6.2 months (range 1 day to 15.3 months) with a median of nine doses (range 1 to 23). Fifty-one percent of patients were exposed to KEYTRUDA for greater than 6 months and 21% for greater than 1 year. KEYTRUDA was discontinued for adverse reactions in 6% of the 89 patients.The most common adverse reactions (reported in at least 20% of patients) were fatigue, cough, nausea, pruritus, rash, decreased appetite, constipation, arthralgia, and diarrhea.
Other clinically important adverse reactions observed in up to 10% of patients treated with KEYTRUDA were: Infections and infestations: sepsis
As with all therapeutic proteins, there is the potential for immunogenicity. Because trough levels of pembrolizumab interfere with the electrochemiluminescent (ECL) assay results, a subset analysis was performed in the patients with a concentration of pembrolizumab below the drug tolerance level of the anti-product antibody assay. In this analysis, none of the 97 patients who were treated with 2 mg/kg every 3 weeks tested positive for treatment-emergent anti-pembrolizumab antibodies. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of incidence of antibodies to KEYTRUDA with the incidences of antibodies to other products may be misleading. 7 DRUG INTERACTIONS No formal pharmacokinetic drug interaction studies have been conducted with KEYTRUDA. 8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Pregnancy Category D. Risk Summary Based on its mechanism of action, KEYTRUDA may cause fetal harm when administered to a pregnant woman. Animal models link the PD-1/PDL-1 signaling pathway with maintenance of pregnancy through induction of maternal immune tolerance to fetal tissue. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus. Animal Data Animal reproduction studies have not been conducted with KEYTRUDA to evaluate its effect on reproduction and fetal development, but an assessment of the effects on reproduction was provided. A central function of the PD-1/PD-L1 pathway is to preserve pregnancy by maintaining maternal immune tolerance to the fetus. Blockade of PD-L1 signaling has been shown in murine models of pregnancy to disrupt tolerance to the fetus and to result in an increase in fetal loss; therefore, potential risks of administering KEYTRUDA during pregnancy include increased rates of abortion or stillbirth. As reported in the literature, there were no malformations related to the blockade of PD-1 signaling in the offspring of these animals; however, immune-mediated disorders occurred in PD-1 knockout mice. Human IgG4 (immunoglobulins) are known to cross the placenta; therefore, pembrolizumab has the potential to be transmitted from the mother to the developing fetus. Based on its mechanism of action, fetal exposure to pembrolizumab may increase the risk of developing immune-mediated disorders or of altering the normal immune response. 8.3 Nursing Mothers It is not known whether KEYTRUDA is excreted in human milk. No studies have been conducted to assess the impact of KEYTRUDA on milk production or its presence in breast milk. Because many drugs are excreted in human milk, instruct women to discontinue nursing during treatment with KEYTRUDA. 8.4 Pediatric Use Safety and effectiveness of KEYTRUDA have not been established in pediatric patients. 8.5 Geriatric Use Of the 411 patients treated with KEYTRUDA, 39% were 65 years and over. No overall differences in safety or efficacy were reported between elderly patients and younger patients. 8.6 Renal Impairment Based on a population pharmacokinetic analysis, no dose adjustment is needed for patients with renal impairment [see Clinical Pharmacology (12.3)]. 8.7 Hepatic Impairment Based on a population pharmacokinetic analysis, no dose adjustment is needed for patients with mild hepatic impairment [total bilirubin (TB) less than or equal to ULN and AST greater than ULN or TB greater than 1 to 1.5 times ULN and any AST]. KEYTRUDA has not been studied in patients with moderate (TB greater than 1.5 to 3 times ULN and any AST) or severe (TB greater than 3 times ULN and any AST) hepatic impairment [see Clinical Pharmacology (12.3)]. 8.8 Females and Males of Reproductive Potential Based on its mechanism of action, KEYTRUDA may cause fetal harm when administered to a pregnant woman [see Warnings and Precautions (5.8) and Use in Specific Populations (8.1)]. Advise females of reproductive potential to use highly effective contraception during treatment with KEYTRUDA and for at least 4 months following the last dose of pembrolizumab. 10 OVERDOSAGE There is no information on overdosage with KEYTRUDA. 11 DESCRIPTION Pembrolizumab is a humanized monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD-L1 and PD-L2. Pembrolizumab is an IgG4 kappa immunoglobulin with an approximate molecular weight of 149 kDa. KEYTRUDA is a sterile, preservative-free, white to off-white lyophilized powder in single-use vials. Each vial is reconstituted and diluted for intravenous infusion. Each 2 mL of reconstituted solution contains 50 mg of pembrolizumab and is formulated in L-histidine (3.1 mg), polysorbate-80 (0.4 mg), sucrose (140 mg). May contain hydrochloric acid/sodium hydroxide to adjust pH to 5.5. 12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Binding of the PD-1 ligands, PD-L1 and PD-L2, to the PD-1 receptor found on T cells, inhibits T cell proliferation and cytokine production. Upregulation of PD-1 ligands occurs in some tumors and signaling through this pathway can contribute to inhibition of active T-cell immune surveillance of tumors. Pembrolizumab is a monoclonal antibody that binds to the PD-1 receptor and blocks its interaction with PD-L1 and PD-L2, releasing PD-1 pathway-mediated inhibition of the immune response, including the anti-tumor immune response. In syngeneic mouse tumor models, blocking PD-1 activity resulted in decreased tumor growth. 12.3 Pharmacokinetics The pharmacokinetics of pembrolizumab was studied in 479 patients who received doses of 1 to 10 mg/kg every 2 weeks or 2 to 10 mg/kg every 3 weeks. Based on a population pharmacokinetic analysis, the mean [% coefficient of variation (CV%)] clearance (CL) is 0.22 L/day (28%) and the mean (CV%) elimination half-life (t1/2) is 26 days (24%). Steady-state concentrations of pembrolizumab were reached by 18 weeks of repeated dosing with an every 3-week regimen and the systemic accumulation was 2.1-fold. The peak concentration (Cmax), trough concentration (Cmin), and area under the plasma concentration versus time curve at steady state (AUCss) of pembrolizumab increased dose proportionally in the dose range of 2 to 10 mg/kg every 3 weeks. Specific Populations: The effects of various covariates on the pharmacokinetics of pembrolizumab were assessed in population pharmacokinetic analyses. The CL of pembrolizumab increased with increasing body weight; the resulting exposure differences were adequately addressed by the administration of a weight-based dose. The following factors had no clinically important effect on the CL of pembrolizumab: age (range 18-94 years), gender, renal impairment, mild hepatic impairment, and tumor burden. The effect of race could not be assessed due to limited data available in non-White patients. Renal Impairment: The effect of renal impairment on the CL of pembrolizumab was evaluated by population pharmacokinetic analyses in patients with mild (eGFR 60 to 89 mL/min/1.73 m2; n=210), moderate (eGFR 30 to 59 mL/min/1.73m2; n=43), or severe (eGFR 15 to 29 mL/min/1.73m2; n=2) renal impairment compared to patients with normal (eGFR greater than or equal to 90 mL/min/1.73m2; n=221) renal function. No clinically important differences in the CL of pembrolizumab were found between patients with renal impairment and patients with normal renal function [see Use in Specific Populations (8.6)]. Hepatic Impairment: The effect of hepatic impairment on the CL of pembrolizumab was evaluated by population pharmacokinetic analyses in patients with mild hepatic impairment (TB less than or equal to ULN and AST greater than ULN or TB between 1 and 1.5 times ULN and any AST; n=59) compared to patients with normal hepatic function (TB and AST less than or equal to ULN; n=410). No clinically important differences in the CL of pembrolizumab were found between patients with mild hepatic impairment and normal hepatic function. KEYTRUDA has not been studied in patients with moderate (TB greater than 1.5 to 3 times ULN and any AST) or severe (TB greater than 3 times ULN and any AST) hepatic impairment [see Use in Specific Populations (8.7)]. 13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility No studies have been performed to test the potential of pembrolizumab for carcinogenicity or genotoxicity. Fertility studies have not been conducted with pembrolizumab. In 1-month and 6-month repeat-dose toxicology studies in monkeys, there were no notable effects in the male and female reproductive organs; however, most animals in these studies were not sexually mature. 13.2 Animal Toxicology and/or Pharmacology In animal models, inhibition of PD-1 signaling resulted in an increased incidence of infections and enhanced inflammatory responses. M. tuberculosis-infected PD-1 knockout mice exhibit markedly decreased survival compared with wild-type controls, which correlated with increased bacterial proliferation and inflammatory responses in these animals. PD-1 knockout mice have also shown decreased survival following infection with lymphocytic choriomeningitis virus (LCMV). Administration of pembrolizumab in chimpanzees with naturally occurring chronic hepatitis B infection resulted in two out of four animals with significantly increased levels of serum ALT, AST, and GGT, which persisted for at least 1 month after discontinuation of pembrolizumab. 14 CLINICAL STUDIES The efficacy of KEYTRUDA was investigated in a multicenter, open-label, randomized (1:1), dose-comparative, activity-estimating cohort of Trial 1. Key eligibility criteria were unresectable or metastatic melanoma with progression of disease; refractory to two or more doses of ipilimumab (3 mg/kg or higher) and, if BRAF V600 mutation-positive, a BRAF or MEK inhibitor; and disease progression within 24 weeks following the last dose of ipilimumab. The trial excluded patients with autoimmune disease; a medical condition that required immunosuppression; and a history of severe immune-mediated adverse reactions with ipilimumab, defined as any Grade 4 toxicity requiring treatment with corticosteroids or Grade 3 toxicity requiring corticosteroid treatment (greater than 10 mg/day prednisone or equivalent dose) for greater than 12 weeks. Patients were randomized to receive 2 mg/kg (n=89) or 10 mg/kg (n=84) of KEYTRUDA every 3 weeks until unacceptable toxicity or disease progression that was symptomatic, was rapidly progressive, required urgent intervention, occurred with a decline in performance status, or was confirmed at 4 to 6 weeks with repeat imaging. Assessment of tumor status was performed every 12 weeks. The major efficacy outcome measures were confirmed overall response rate (ORR) according to Response Evaluation Criteria in Solid Tumors (RECIST 1.1) as assessed by blinded independent central review and duration of response. Among the 173 patients enrolled, the median age was 61 years (36% age 65 or older); 60% male; 97% White; and 66% and 34% with an ECOG performance status 0 and 1, respectively. Disease characteristics were BRAF V600 mutation (17%), elevated lactate dehydrogenase (39%), M1c (82%), brain metastases (9%), and two or more prior therapies for advanced or metastatic disease (73%). The ORR was 24% (95% confidence interval: 15, 34) in the 2 mg/kg arm, consisting of 1 complete response and 20 partial responses. Among the 21 patients with an objective response, 3 (14%) had progression of disease 2.8, 2.9, and 8.2 months after initial response. The remaining 18 patients (86%) had ongoing responses with durations ranging from 1.4+ to 8.5+ months, which included 8 patients with ongoing responses of 6 months or longer. One additional patient developed two new asymptomatic lesions at the first tumor assessment concurrent with a 75% decrease in overall tumor burden; KEYTRUDA was continued and this reduction in tumor burden was durable for 5+ months. There were objective responses in patients with and without BRAF V600 mutation-positive melanoma. Similar ORR results were observed in the 10 mg/kg arm. 16 HOW SUPPLIED/STORAGE AND HANDLING KEYTRUDA is supplied in a carton containing one 50 mg single-use vial (NDC 0006-3029-02). Store vials under refrigeration at 2°C to 8°C (36°F to 46°F). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
KEYTRUDA(pembrolizumab)注射剂简介:
KEYTRUDA(pembrolizumab) injection, powder, lyophilized, for solution [Merck Sharp & Dohme Corp.] 第一个PD-1阻断药接受监管局批准,授权加速批准批准日期:2014年9月4日剂量和给药方法推荐给药KEY ... 责任编辑:admin |
最新文章更多推荐文章更多热点文章更多
|