|
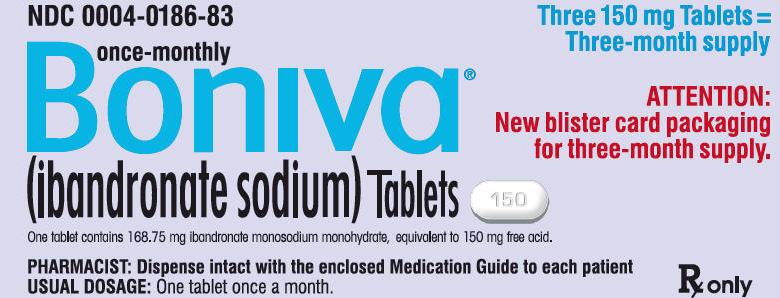
英文药名: Boniva(ibandronate sodium tablets) 中文药名: 伊班膦酸钠片 生产厂家: 基因泰克公司[罗氏]
One 150 mg tablet taken once monthly or one 2.5 mg tablet taken once daily (2.1) Dosing instructions (2.2) Swallow whole tablet with 6-8 oz of plain water only, at least 60 minutes before the first food, beverage, or medication of the day. Do not lie down for at least 60 minutes after taking BONIVA. Do not eat, drink (except for water), or take other medication for 60 minutes after taking BONIVA. DOSAGE FORMS AND STRENGTHS Tablets: 2.5mg, 150mg (3) CONTRAINDICATIONS Abnormalities of the esophagus which delay esophageal emptying such as stricture or achalasia (4, 5.1) Inability to stand or sit upright for at least 60 minutes (4, 5.1) Hypocalcemia (4) Hypersensitivity to BONIVA (4) WARNINGS AND PRECAUTIONS Severe irritation of the upper gastrointestinal (GI) mucosa can occur. Dosing instructions should be followed and caution should be used in patients with active upper GI disease. Discontinue use if new or worsening symptoms occur. (5.1) Hypocalcemia may worsen during treatment. Correct hypocalcemia before use. (5.2) Severe bone, joint, and muscle pain may occur. Consider discontinuing use if symptoms develop. (5.3) Osteonecrosis of the jaw has been reported. (5.4) ADVERSE REACTIONS The most common adverse reactions (>5%) are back pain, dyspepsia, pain in extremity, diarrhea, headache, and myalgia. (6) To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS Calcium supplements, antacids and some oral medications may interfere with absorption of ibandronate. (7.1) Use caution when co-prescribing aspirin/nonsteroidal anti-inflammatory drugs that may worsen gastrointestinal irritation. (7.2) USE IN SPECIFIC POPULATIONS BONIVA is not recommended in patients with severe renal impairment (creatinine clearance <30 mL/min). (5.5, 8.6) See 17 for PATIENT COUNSELING INFORMATION. Revised: 12/2010 FULL PRESCRIBING INFORMATION: CONTENTS* 1 INDICATIONS AND USAGE Enter section text here 1.1 Treatment and Prevention of Postmenopausal Osteoporosis BONIVA is indicated for the treatment and prevention of osteoporosis in postmenopausal women. BONIVA increases bone mineral density (BMD) and reduces the incidence of vertebral fractures. 2 DOSAGE AND ADMINISTRATION Enter section text here 2.1 Dose The dose of BONIVA is either one 150 mg tablet taken once monthly on the same date each month or one 2.5 mg tablet taken once daily. 2.2 Dosing Instructions To maximize absorption and clinical benefit, BONIVA should be taken at least 60 minutes before the first food or drink (other than water) of the day or before taking any oral medication or supplementation, including calcium, antacids, or vitamins (see DRUG INTERACTIONS [7.1]). To facilitate delivery to the stomach and thus reduce the potential for esophageal irritation, BONIVA tablets should be swallowed whole with a full glass of plain water (6 to 8 oz) while the patient is standing or sitting in an upright position. Patients should not lie down for 60 minutes after taking BONIVA (see WARNINGS AND PRECAUTIONS [5.1]). Patients should not eat, drink anything except water, or take other medications for at least 60 minutes after taking BONIVA. Plain water is the only drink that should be taken with BONIVA. Note that some mineral waters may have a higher concentration of calcium and therefore should not be used. Patients should not chew or suck the tablet because of a potential for oropharyngeal ulceration. The BONIVA 150 mg tablet should be taken on the same date each month (i.e., the patient's BONIVA day). The patient must not take two 150 mg tablets within the same week. If the once-monthly dose is missed, and the patient's next scheduled BONIVA day is more than 7 days away, the patient should be instructed to take one BONIVA 150 mg tablet in the morning following the date that it is remembered. The patient should then return to taking one BONIVA 150 mg tablet every month in the morning of their chosen day, according to their original schedule. If the once-monthly dose is missed, and the patient's next scheduled BONIVA day is only 1 to 7 days away, the patient must wait until the subsequent month's scheduled BONIVA day to take their tablet. The patient should then return to taking one BONIVA 150 mg tablet every month in the morning of their chosen day, according to their original schedule. 2.3 Recommendations for Calcium and Vitamin D Supplementation Patients should receive supplemental calcium and vitamin D if dietary intake is inadequate (see DRUG INTERACTIONS [7.1]). 2.4 use in Specific Populations BONIVA is not recommended for use in patients with severe renal impairment (creatinine clearance of <30 mL/min). No dose adjustment is necessary for patients with mild or moderate renal impairment. No dose adjustment is necessary for the elderly, or for patients with hepatic impairment. 3 DOSAGE FORMS AND STRENGTHS Tablets, 2.5 mg and 150 mg 4 CONTRAINDICATIONS Abnormalities of the esophagus which delay esophageal emptying such as stricture or achalasia (see Upper Gastrointestinal Adverse Reactions [5.1]) Inability to stand or sit upright for at least 60 minutes (see Dosing Instructions [2.2], Upper Gastrointestinal Adverse Reactions [5.1]) Hypocalcemia (see WARNINGS AND PRECAUTIONS [5.2]) Known hypersensitivity to BONIVA or to any of its excipients (see ADVERSE REACTIONS [6.2]). 5 WARNINGS AND PRECAUTIONS Enter section text here 5.1 Upper Gastrointestinal Adverse Reactions BONIVA, like other bisphosphonates administered orally, may cause local irritation of the upper gastrointestinal mucosa. Because of these possible irritant effects and a potential for worsening of the underlying disease, caution should be used when BONIVA is given to patients with active upper gastrointestinal problems (such as known Barrett's esophagus, dysphagia, other esophageal diseases, gastritis, duodenitis or ulcers). Esophageal adverse experiences, such as esophagitis, esophageal ulcers and esophageal erosions, occasionally with bleeding and rarely followed by esophageal stricture or perforation, have been reported in patients receiving treatment with oral bisphosphonates. In some cases, these have been severe and required hospitalization. Physicians should therefore be alert to any signs or symptoms signaling a possible esophageal reaction and patients should be instructed to discontinue BONIVA and seek medical attention if they develop dysphagia, odynophagia, retrosternal pain or new or worsening heartburn. The risk of severe esophageal adverse experiences appears to be greater in patients who lie down after taking oral bisphosphonates and/or who fail to swallow it with the recommended full glass (6-8 oz) of water, and/or who continue to take oral bisphosphonates after developing symptoms suggestive of esophageal irritation. Therefore, it is very important that the full dosing instructions are provided to, and understood by, the patient (see DOSAGE AND ADMINISTRATION [2.2]). In patients who cannot comply with dosing instructions due to mental disability, therapy with BONIVA should be used under appropriate supervision. There have been post-marketing reports of gastric and duodenal ulcers with oral bisphosphonate use, some severe and with complications, although no increased risk was observed in controlled clinical trials. 5.2 Hypocalcemia and Mineral Metabolsim Treat hypocalcemia and other disturbances of bone and mineral metabolism before starting BONIVA therapy. Adequate intake of calcium and vitamin D is important in all patients to prevent hypocalcemia (see DOSAGE AND ADMINISTRATION [2.3]). Hypocalcemia following dosing has been reported postmarketing. 5.3 Musculoskeletal Pain Severe and occasionally incapacitating bone, joint, and/or muscle pain has been reported in patients taking BONIVA and other bisphosphonates (see ADVERSE REACTIONS [6]). The time to onset of symptoms varied from one day to several months after starting the drug. Most patients had relief of symptoms after stopping. A subset had recurrence of symptoms when rechallenged with the same drug or another bisphosphonate. Consider discontinuing use if severe symptoms develop. 5.4 Jaw Osteonecrosis Osteonecrosis, primarily in the jaw, has been reported in patients treated with bisphosphonates. Most cases have been in cancer patients undergoing dental procedures, but some have occurred in patients with postmenopausal osteoporosis or other diagnoses. Known risk factors for osteonecrosis include a diagnosis of cancer, concomitant therapies (e.g., chemotherapy, radiotherapy, corticosteroids), and co-morbid disorders (e.g., anemia, coagulopathy, infection, pre-existing dental disease). Most reported cases have been in patients treated with bisphosphonates intravenously but some have been in patients treated orally (see ADVERSE REACTIONS [6.2]). For patients who develop osteonecrosis of the jaw (ONJ) while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgment of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment. 5.5 Severe Renal Impairment BONIVA is not recommended for use in patients with severe renal impairment (creatinine clearance of <30 mL/min). 6 ADVERSE REACTIONS Enter section text here 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. Treatment and Prevention of Postmenopausal Osteoporosis Daily Dosing The safety of BONIVA 2.5 mg once daily in the treatment and prevention of postmenopausal osteoporosis was assessed in 3577 patients aged 41 – 82 years. The duration of the trials was 2 to 3 years, with 1134 patients exposed to placebo and 1140 exposed to BONIVA 2.5 mg. Patients with pre-existing gastrointestinal disease and concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors and H2 antagonists were included in these clinical trials. All patients received 500 mg calcium plus 400 IU vitamin D supplementation daily. The incidence of all-cause mortality was 1% in the placebo group and 1.2% in the BONIVA 2.5 mg daily group. The incidence of serious adverse events was 20% in the placebo group and 23% in the BONIVA 2.5 mg daily group. The percentage of patients who withdrew from treatment due to adverse events was approximately 17% in both the BONIVA 2.5 mg daily group and the placebo group. Table 1 lists adverse events from the treatment and prevention studies reported in ≥2% of patients and more frequently in patients treated daily with BONIVA than patients treated with placebo. Table 1 Adverse Events Occurring at a Frequency ≥2% and More Frequently in Patients Treated with BONIVA than in Patients Treated with Placebo Daily in the Osteoporosis Treatment and Prevention Studies
The incidence of adverse events in the placebo and BONIVA 2.5 mg daily groups were: dyspepsia (10% vs. 12%), diarrhea (5% vs. 7%), and abdominal pain (5% vs. 6%). Musculoskeletal Adverse Events The incidence of adverse events in the placebo and BONIVA 2.5 mg daily groups were: back pain (12% vs. 14%), arthralgia (14% vs. 14%) and myalgia (5% vs. 6%). Ocular Adverse Events Reports in the medical literature indicate that bisphosphonates may be associated with ocular inflammation such as iritis and scleritis. In some cases, these events did not resolve until the bisphosphonate was discontinued. There were no reports of ocular inflammation in studies with BONIVA 2.5 mg daily. Monthly Dosing The safety of BONIVA 150 mg once monthly in the treatment of postmenopausal osteoporosis was assessed in a two year trial which enrolled 1583 patients aged 54 – 81 years, with 395 patients exposed to BONIVA 2.5 mg daily and 396 exposed to BONIVA 150 mg monthly. Patients with active or significant pre-existing gastrointestinal disease were excluded from this trial. Patients with dyspepsia or concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors and H2 antagonists were included in this study. All patients received 500 mg calcium plus 400 IU vitamin D supplementation daily. After one year, the incidence of all-cause mortality was 0.3% in both the BONIVA 2.5 mg daily group and the BONIVA 150 mg monthly group. The incidence of serious adverse events was 5% in the BONIVA 2.5 mg daily group and 7% in the BONIVA 150 mg monthly group. The percentage of patients who withdrew from treatment due to adverse events was 9% in the BONIVA 2.5 mg daily group and 8% in the BONIVA 150 mg monthly group. Table 2 lists the adverse events reported in ≥2% of patients. Table 2 Adverse Events with an Incidence of at Least 2% in Patients Treated with BONIVA 2.5 mg Daily or 150 mg Once-Monthly for Treatment of Postmenopausal Osteoporosis
Combination of influenza-like illness and acute phase reaction Combination of rash pruritic, rash macular, rash papular, rash generalized, rash erythematous, dermatitis, dermatitis allergic, dermatitis medicamentosa, erythema and exanthem Gastrointestinal Adverse Events The incidence of adverse events in the BONIVA 2.5 mg daily and BONIVA 150 mg monthly groups were: dyspepsia (7% vs. 6%), diarrhea (4% vs. 5%), and abdominal pain (5% vs. 8%). Musculoskeletal Adverse Events The incidence of adverse events in the BONIVA 2.5 mg daily and BONIVA 150 mg monthly groups were: back pain (4% vs. 5%), arthralgia (4% vs. 6%) and myalgia (1% vs. 2%). Acute Phase Reactions Symptoms consistent with acute phase reactions have been reported with bisphosphonate use. Over the two years of the study, the overall incidence of acute phase reaction symptoms was 3% in the BONIVA 2.5 mg daily group and 9% in the BONIVA 150 mg monthly group. These incidence rates are based on the reporting of any of 33 acute-phase reaction like symptoms within 3 days of the monthly dosing and lasting 7 days or less. Influenza like illness was reported in no patients in the BONIVA 2.5 mg daily group and 2% in the BONIVA 150 mg monthly group. Ocular Adverse Events Two patients who received BONIVA 150 mg once-monthly experienced ocular inflammation, one was a case of uveitis and the other scleritis. One hundred sixty (160) postmenopausal women without osteoporosis participated in a 1-year, double-blind, placebo-controlled study of BONIVA 150 mg once-monthly for prevention of bone loss. Seventy-seven subjects received BONIVA and 83 subjects received placebo. The overall pattern of adverse events was similar to that previously observed. 6.2 Postmarketing Experience The following adverse reactions have been identified during postapproval use of BONIVA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Hypersensitivity Allergic reactions including anaphylaxis, angioedema, bronchospasm and rash have been reported (see CONTRAINDICATIONS [4]). Hypocalcemia Hypocalcemia has been reported in patients treated with BONIVA (see WARNINGS AND PRECAUTIONS [5.2]). Musculoskeletal Pain Bone, joint, or muscle pain (musculoskeletal pain), described as severe or incapacitating, has been reported (see WARNINGS AND PRECAUTIONS [5.3]). Jaw Osteonecrosis Osteonecrosis of the jaw has been reported in patients treated with BONIVA (see WARNINGS AND PRECAUTIONS [5.4]). 7 DRUG INTERACTIONS Enter section text here 7.1 Calcium Supplements/Antacids Products containing calcium and other multivalent cations (such as aluminum, magnesium, iron) are likely to interfere with absorption of BONIVA. BONIVA should be taken at least 60 minutes before any oral medications, including medications containing multivalent cations (such as antacids, supplements or vitamins). Also, patients should wait at least 60 minutes after dosing before taking any other oral medications (see PATIENT COUNSELING INFORMATION [17.1]). 7.2 Aspirin/Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) Because aspirin, NSAIDs, and bisphosphonates are all associated with gastrointestinal irritation, caution should be exercised in the concomitant use of aspirin or NSAIDs with BONIVA. 7.3 H2 Blockers In healthy volunteers, co-administration with ranitidine resulted in a 20% increased bioavailability of ibandronate, which was not considered to be clinically relevant (see CLINICAL PHARMACOLOGY [12.3]). 7.4 Drug/Laboratory Test Interactions Bisphosphonates are known to interfere with the use of bone-imaging agents. Specific studies with ibandronate have not been performed. 8 USE IN SPECIFIC POPULATIONS Enter section text here 8.1 Pregnancy: Category C There are no adequate and well-controlled studies in pregnant women. BONIVA should be used during pregnancy only if the potential benefit justifies the potential risk to the mother and fetus. Bisphosphonates are incorporated into the bone matrix, from where they are gradually released over periods of weeks to years. The extent of bisphosphonate incorporation into adult bone, and hence, the amount available for release back into the systemic circulation, is directly related to the total dose and duration of bisphosphonate use. Although there are no data on fetal risk in humans, bisphosphonates do cause fetal harm in animals, and animal data suggest that uptake of bisphosphonates into fetal bone is greater than into maternal bone. Therefore, there is a theoretical risk of fetal harm (e.g., skeletal and other abnormalities) if a woman becomes pregnant after completing a course of bisphosphonate therapy. The impact of variables such as time between cessation of bisphosphonate therapy to conception, the particular bisphosphonate used, and the route of administration (intravenous versus oral) on this risk has not been established. In female rats given ibandronate orally at doses ≥3 times human exposure at the recommended daily oral dose of 2.5 mg or ≥1 times human exposure at the recommended once-monthly oral dose of 150 mg beginning 14 days before mating and continuing through lactation, maternal deaths were observed at the time of delivery in all dose groups. Perinatal pup loss in dams given 45 times human exposure at the recommended daily dose and 13 times the recommended once-monthly dose was likely related to maternal dystocia. Calcium supplementation did not completely prevent dystocia and periparturient mortality in any of the treated groups at ≥16 times the recommended daily dose and ≥4.6 times the recommended once-monthly dose. A low incidence of postimplantation loss was observed in rats treated from 14 days before mating throughout lactation or during gestation, only at doses causing maternal dystocia and periparturient mortality. In pregnant rats dosed orally from gestation day 17 through lactation day 21 (following closure of the hard palate through weaning), maternal toxicity, including dystocia and mortality, fetal perinatal and postnatal mortality, were observed at doses equivalent to human exposure at the recommended daily and ≥4 times the recommended once-monthly dose. Periparturient mortality has also been observed with other bisphosphonates and appears to be a class effect related to inhibition of skeletal calcium mobilization resulting in hypocalcemia and dystocia (see NONCLINICAL TOXICOLOGY [13.2]). Exposure of pregnant rats during the period of organogenesis resulted in an increased fetal incidence of RPU (renal pelvis ureter) syndrome at oral doses 30 times the human exposure at the recommended daily oral dose of 2.5 mg and ≥9 times the recommended once-monthly oral dose of 150 mg. Impaired pup neuromuscular development (cliff avoidance test) was observed at 45 times human exposure at the daily dose and 13 times the once-monthly dose (see NONCLINICAL TOXICOLOGY [13.2]). In pregnant rabbits treated orally with ibandronate during gestation at doses ≥8 times the recommended human daily oral dose of 2.5 mg and ≥4 times the recommended human once-monthly oral dose of 150 mg, dose-related maternal mortality was observed in all treatment groups. The deaths occurred prior to parturition and were associated with lung edema and hemorrhage. No significant fetal anomalies were observed (see NONCLINICAL TOXICOLOGY [13.2]). 8.3 Nursing Mothers It is not known whether BONIVA is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when BONIVA is administered to a nursing woman. In lactating rats treated with intravenous doses, ibandronate was present in breast milk from 2 to 24 hours after dose administration. Concentrations in milk averaged 1.5 times plasma concentrations. 8.4 Pediatric Use Safety and effectiveness in pediatric patients have not been established. 8.5 Geriatric Use Of the patients receiving BONIVA 2.5 mg daily in postmenopausal osteoporosis studies, 52% were over 65 years of age, and 10% were over 75 years of age. Of the patients receiving BONIVA 150 mg once-monthly in the postmenopausal osteoporosis 1-year study, 52% were over 65 years of age, and 9% were over 75 years of age. No overall differences in effectiveness or safety were observed between these patients and younger patients but greater sensitivity in some older individuals cannot be ruled out. 8.6 Renal Impairment BONIVA is not recommended for use in patients with severe renal impairment (creatinine clearance <30 mL/min). 10 OVERDOSAGE No specific information is available on the treatment of overdosage of BONIVA. However, based on knowledge of this class of compounds, oral overdosage may result in hypocalcemia, hypophosphatemia, and upper gastrointestinal adverse events, such as upset stomach, dyspepsia, esophagitis, gastritis, or ulcer. Milk or antacids should be given to bind BONIVA. Due to the risk of esophageal irritation, vomiting should not be induced, and the patient should remain fully upright. Dialysis would not be beneficial. 11 DESCRIPTION BONIVA (ibandronate sodium) is a nitrogen-containing bisphosphonate that inhibits osteoclast-mediated bone resorption. The chemical name for ibandronate sodium is 3-(N-methyl-N-pentyl) amino-1-hydroxypropane-1,1-diphosphonic acid, monosodium salt, monohydrate with the molecular formula C9H22NO7P2Na•H2O and a molecular weight of 359.24. Ibandronate sodium is a white- to off-white powder. It is freely soluble in water and practically insoluble in organic solvents. Ibandronate sodium has the following structural formula:
BONIVA 2.5 mg daily did not reduce the incidence of nonvertebral fractures (secondary efficacy measure). There was a similar number of nonvertebral osteoporotic fractures at 3 years reported in women treated with BONIVA 2.5 mg daily [9.1%, (95% CI: 7.1%, 11.1%)] and placebo [8.2%, (95% CI: 6.3%, 10.2%)]. The two treatment groups were also similar with regard to the number of fractures reported at the individual nonvertebral sites: pelvis, femur, wrist, forearm, rib, and hip. Bone Mineral Density (BMD) BONIVA significantly increased BMD at the lumbar spine and hip relative to treatment with placebo. In the 3-year osteoporosis treatment study, BONIVA 2.5 mg daily produced increases in lumbar spine BMD that were progressive over 3 years of treatment and were statistically significant relative to placebo at 6 months and at all later time points. Lumbar spine BMD increased by 6.4% after 3 years of treatment with 2.5 mg daily BONIVA compared with 1.4% in the placebo group. Table 4 displays the significant increases in BMD seen at the lumbar spine, total hip, femoral neck, and trochanter compared to placebo. Thus, overall BONIVA reverses the loss of BMD, a central factor in the progression of osteoporosis. Table 4 Mean Percent Change in BMD from Baseline to Endpoint in Patients Treated Daily with BONIVA 2.5 mg or Placebo in the 3-Year Osteoporosis Treatment Study*
Bone Histology The effects of BONIVA 2.5 mg daily on bone histology were evaluated in iliac crest biopsies from 16 women after 22 months of treatment and 20 women after 34 months of treatment. The histological analysis of bone biopsies showed bone of normal quality and no indication of osteomalacia or a mineralization defect. Once-Monthly Dosing The effectiveness and safety of BONIVA once-monthly were demonstrated in a randomized, double-blind, multinational, noninferiority trial in 1602 women aged 54 to 81 years, who were on average 18 years postmenopause, and had L2-L4 lumbar spine BMD T-score below -2.5 SD at baseline. The main outcome measure was the comparison of the percentage change from baseline in lumbar spine BMD after 1 year of treatment with once-monthly ibandronate (100 mg, 150 mg) to daily ibandronate (2.5 mg). All patients received 400 IU vitamin D and 500 mg calcium supplementation per day. BONIVA 150 mg once-monthly (n=327) was shown to be noninferior to BONIVA 2.5 mg daily (n=318) in lumbar spine BMD in a 1-year, double-blind, multicenter study of women with postmenopausal osteoporosis. In the primary efficacy analysis (per-protocol population), the mean increases from baseline in lumbar spine BMD at 1 year were 3.86% (95% CI: 3.40%, 4.32%) in the 2.5 mg daily group and 4.85% (95% CI: 4.41%, 5.29%) in the 150 mg once-monthly group; the mean difference between 2.5 mg daily and 150 mg once-monthly was 0.99% (95% CI: 0.38%, 1.60%), which was statistically significant (p=0.002). The results of the intent-to-treat analysis were consistent with the primary efficacy analysis. The 150 mg once-monthly group also had consistently higher BMD increases at the other skeletal sites compared to the 2.5 mg daily group. 14.2 Prevention of Postmenopausal Osteoporosis Daily Dosing The safety and effectiveness of BONIVA 2.5 mg daily for the prevention of postmenopausal osteoporosis were demonstrated in a randomized, double-blind, placebo-controlled 2-year study (Prevention Study) of 653 postmenopausal women without osteoporosis at baseline. Women were aged 41 to 82 years, were on average 8.5 years postmenopause, and had lumbar spine BMD T-scores >-2.5. Women were stratified according to time since menopause (1 to 3 years, >3 years) and baseline lumbar spine BMD (T-score: >-1, -1 to -2.5). The study compared daily BONIVA at three dose levels (0.5 mg, 1.0 mg, 2.5 mg) with placebo. All women received 500 mg of supplemental calcium per day. The primary efficacy measure was the change in BMD of lumbar spine after 2 years of treatment. BONIVA 2.5 mg daily resulted in a mean increase in lumbar spine BMD of 3.1% compared with placebo following 2 years of treatment. Increases in BMD were seen at 6 months and at all later time points. Irrespective of the time since menopause or the degree of pre-existing bone loss, treatment with BONIVA resulted in a higher BMD response at the lumbar spine compared with placebo across all four baseline strata [time since menopause (1 to 3 years, >3 years) and baseline lumbar spine BMD (T-score: >-1, -1 to -2.5)]. Compared with placebo, treatment with BONIVA 2.5 mg daily increased BMD of the total hip by 1.8%, the femoral neck by 2.0%, and the trochanter by 2.1%. Once-Monthly Dosing BONIVA 150 mg once-monthly prevented bone loss in a majority (88.2%) of women in a randomized, double-blind, placebo-controlled 1-year study (Monthly Prevention Study) of 160 postmenopausal women with low bone mass at baseline (T-score of -1 to -2.5). Women, aged 46 to 60 years, were on average 5.4 years postmenopause. All women received 400 IU of vitamin D and 500 mg calcium supplementation daily. The primary efficacy measure was the relative change in BMD at the lumbar spine after 1 year of treatment. BONIVA 150 mg once-monthly resulted in a mean increase in lumbar spine BMD of 4.12% (95% confidence interval 2.96 – 5.28) compared with placebo following 1 year of treatment (p<0.0001), based on a 3.73% and -0.39% mean change in BMD from baseline in the 150 mg once-monthly BONIVA and placebo treatment groups, respectively. BMD at other skeletal sites was also increased relative to baseline values. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d6d7711f-541b-47d1-b937-2c6a021eb6c3#footnote-reference-4 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||