| 【药物名称】 中文通用名称:酒石酸美托洛尔 英文通用名称:Metoprolol Tartrate 其它名称:倍他乐克、伯他乐安、甲氧乙心安、酒石酸美多心安、美多洛尔、美多心安、美他新、美托洛尔、蒙得康、素可丁、托西尔康、Betaloc、Lopreser、Lopresor、Lopressor、Metoprolol、Metoprololum、Seloken、Toprol、VasocardinF 【临床应用】 【药理】 【注意事项】 【不良反应】 【药物相互作用】 【给药说明】 【用法与用量】 【制剂与规格】 【原产地英文商品名】LOPRESSOR HCT (50/25)mg/tab 100tabs/bottle Lopressor HCT® metoprolol tartrate USP and hydrochlorothiazide USP 50/25 Tablets 100/25 Tablets 100/50 Tablets Beta Blocker/Diuretic Antihypertensive Rx only Prescribing Information DESCRIPTION
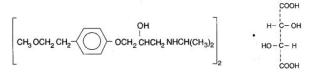
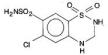
Metoprolol tartrate USP is a white, crystalline powder. It is very soluble in water; freely soluble in methylene chloride, in chloroform, and in alcohol; slightly soluble in acetone; and insoluble in ether. Its molecular weight is 684.82. Hydrochlorothiazide is 6-chloro-3, 4-dihydro-2 H-1,2,4-benzothiadiazine-7- sulfonamide 1,1-dioxide, and its structural formula is
Hydrochlorothiazide USP is a white, or practically white, practically odorless, crystalline powder. It is freely soluble in sodium hydroxide solution, in n-butylamine, and in dimethylformamide; sparingly soluble in methanol; slightly soluble in water; and insoluble in ether, in chloroform, and in dilute mineral acids. Its molecular weight is 297.73. Inactive Ingredients: Cellulose compounds, colloidal silicon dioxide, D&C Yellow No. 10 (100/50-mg tablets), FD&C Blue No. 1 (50/25-mg tablets), FD&C Red No. 40 and FD&C Yellow No. 6 (100/25-mg tablets), lactose, magnesium stearate, povidone, sodium starch glycolate, corn starch, stearic acid, and sucrose. CLINICAL PHARMACOLOGYLopressorLopressor is a beta-adrenergic receptor blocking agent. In vitro and in vivo animal studies have shown that it has a preferential effect on beta1 adrenoreceptors, chiefly located in cardiac muscle. This preferential effect is not absolute, however, and at higher doses, Lopressor also inhibits beta2 adrenoreceptors, chiefly located in the bronchial and vascular musculature. Clinical pharmacology studies have confirmed the beta-blocking activity of metoprolol in man, as shown by (1) reduction in heart rate and cardiac output at rest and upon exercise, (2) reduction of systolic blood pressure upon exercise, (3) inhibition of isoproterenol-induced tachycardia, and (4) reduction of reflex orthostatic tachycardia. Relative beta1 selectivity has been confirmed by the following: (1) In normal subjects, Lopressor is unable to reverse the beta2-mediated vasodilating effects of epinephrine. This contrasts with the effect of nonselective (beta1 plus beta2) beta blockers, which completely reverse the vasodilating effects of epinephrine. (2) In asthmatic patients, Lopressor reduces FEV1 and FVC significantly less than a nonselective beta blocker, propranolol at equivalent beta1-receptor blocking doses. Lopressor has no intrinsic sympathomimetic activity and only weak membrane-stabilizing activity. Lopressor crosses the blood-brain barrier and has been reported in the CSF in a concentration 78% of the simultaneous plasma concentration. Animal and human experiments indicate that Lopressor slows the sinus rate and decreases AV nodal conduction. In controlled clinical studies, Lopressor has been shown to be an effective antihypertensive agent when used alone or as concomitant therapy with thiazide-type diuretics, at dosages of 100-450 mg daily. In controlled, comparative, clinical studies, Lopressor has been shown to be as effective an antihypertensive agent as propranolol, methyldopa, and thiazide-type diuretics, and to be equally effective in supine and standing positions. The mechanism of the antihypertensive effects of beta-blocking agents has not been elucidated. However, several possible mechanisms have been proposed: (1) competitive antagonism of catecholamines at peripheral (especially cardiac) adrenergic neuron sites, leading to decreased cardiac output; (2) a central effect leading to reduced sympathetic outflow to the periphery; and (3) suppression of renin activity. PharmacokineticsIn man, absorption of Lopressor is rapid and complete. Plasma levels following oral administration, however, approximate 50% of levels following intravenous administration, indicating about 50% first-pass metabolism. Plasma levels achieved are highly variable after oral administration. Only a small fraction of the drug (about 12%) is bound to human serum albumin. Metoprolol is a racemic mixture of R- and S-enantiomers. Less than 5% of an oral dose of Lopressor is recovered unchanged in the urine; the rest is excreted by the kidneys as metabolites that appear to have no clinical significance. The systemic availability and half-life of Lopressor in patients with renal failure do not differ to a clinically significant degree from those in normal subjects. Consequently, no reduction in dosage is usually needed in patients with chronic renal failure. In elderly subjects with clinically normal renal function, there are no significant differences in Lopressor pharmacokinetics compared to young subjects. Lopressor is extensively metabolized by the cytochrome P450 enzyme system in the liver. The oxidative metabolism of Lopressor is under genetic control with a major contribution of the polymorphic cytochrome P450 isoform 2D6 (CYP2D6). There are marked ethnic differences in the prevalence of the poor metabolizers (PM) phenotype. Approximately 7% of Caucasians and less than 1% Asian are poor metabolizers. Poor CYP2D6 metabolizers exhibit several-fold higher plasma concentrations of Lopressor than extensive metabolizers with normal CYP2D6 activity. The elimination half-life of metoprolol is about 7.5 hours in poor metabolizers and 2.8 hours in extensive metabolizers. However, the CYP2D6 dependent metabolism of Lopressor seems to have little or no effect on safety or tolerability of the drug. None of the metabolites of Lopressor contribute significantly to its beta-blocking effect. PharmacodynamicsSignificant beta-blocking effect (as measured by reduction of exercise heart rate) occurs within 1 hour after oral administration, and its duration is dose-related. For example, a 50% reduction of the maximum registered effect after single oral doses of 20, 50, and 100 mg occurred at 3.3, 5.0, and 6.4 hours, respectively, in normal subjects. After repeated oral dosages of 100 mg twice daily, a significant reduction in exercise systolic blood pressure was evident at 12 hours. There is a linear relationship between the log of plasma levels and reduction of exercise heart rate. However, antihypertensive activity does not appear to be related to plasma levels. Because of variable plasma levels attained with a given dose and lack of a consistent relationship of antihypertensive activity to dose, selection of proper dosage requires individual titration. HydrochlorothiazideThiazides affect the renal tubular mechanism of electrolyte reabsorption. At maximal therapeutic dosage, all thiazides are approximately equal in their diuretic potency. Thiazides increase excretion of sodium and chloride in approximately equivalent amounts. Natriuresis causes a secondary loss of potassium. The mechanism of the antihypertensive effect of thiazides is unknown. Thiazides do not affect normal blood pressure. PharmacokineticsHydrochlorothiazide is rapidly absorbed, as indicated by peak plasma concentrations 1-2.5 hours after oral administration. Plasma levels of the drug are proportional to dose; the concentration in whole blood is 1.6-1.8 times higher than in plasma. Thiazides are eliminated rapidly by the kidney. After oral administration of 25- to 100-mg doses, 72-97% of the dose is excreted in the urine, indicating dose-independent absorption. Hydrochlorothiazide is eliminated from plasma in a biphasic fashion with a terminal half-life of 10-17 hours. Plasma protein binding is 67.9%. Plasma clearance is 15.9-30.0 L/hr; volume of distribution is 3.6-7.8 L/kg. Gastrointestinal absorption of hydrochlorothiazide is enhanced when administered with food. Absorption is decreased in patients with congestive heart failure, and the pharmacokinetics are considerably different in these patients. PharmacodynamicsThe onset of action of thiazides occurs in 2 hours and the peak effect at about 4 hours. The action persists for approximately 6-12 hours. INDICATIONS AND USAGELopressor HCT is indicated for the management of hypertension. This fixed-combination drug is not indicated for initial therapy of hypertension. If the fixed combination represents the dose titrated to the individual patient’s needs, therapy with the fixed combination may be more convenient than with the separate components. CONTRAINDICATIONSLopressorLopressor is contraindicated in sinus bradycardia, heart block greater than first degree, cardiogenic shock, and overt cardiac failure (see WARNINGS). Hypersensitivity to Lopressor and related derivatives, or to any of the excipients; hypersensitivity to other beta blockers (cross sensitivity between beta blockers can occur). Sick-sinus syndrome. Severe peripheral arterial circulatory disorders. HydrochlorothiazideHydrochlorothiazide is contraindicated in patients with anuria or hypersensitivity to this or other sulfonamide-derived drugs (see WARNINGS). WARNINGSLopressorCardiac Failure: Sympathetic stimulation is a vital component supporting circulatory function in congestive heart failure, and beta blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure. In hypertensive patients who have congestive heart failure controlled by digitalis and diuretics, Lopressor should be administered cautiously. In Patients Without a History of Cardiac Failure: Continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of impending cardiac failure, patients should be fully digitalized and/or given a diuretic. The response should be observed closely. If cardiac failure continues, despite adequate digitalization and diuretic therapy, Lopressor should be withdrawn.
Bronchospastic Diseases: PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD, IN GENERAL, NOT RECEIVE BETA BLOCKERS, including Lopressor HCT. Because of its relative beta1 selectivity, however, Lopressor may be used with caution in patients with bronchospastic disease who do not respond to, or cannot tolerate, other antihypertensive treatment. Since beta1 selectivity is not absolute, a beta2-stimulating agent should be administered concomitantly, and the lowest possible dose of Lopressor should be used. In these circumstances it would be prudent initially to administer Lopressor in smaller doses three times daily, instead of larger doses two times daily, to avoid the higher plasma levels associated with the longer dosing interval (see DOSAGE AND ADMINISTRATION). Major Surgery: The necessity or desirability of withdrawing beta-blocking therapy, including Lopressor HCT, prior to major surgery is controversial; the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures. Lopressor, like other beta blockers, is a competitive inhibitor of beta-receptor agonists, and its effects can be reversed by administration of such agents, e.g., dobutamine or isoproterenol. However, such patients may be subject to protracted severe hypotension. Difficulty in restarting and maintaining the heart beat has also been reported with beta blockers. Diabetes and Hypoglycemia: Lopressor should be used with caution in diabetic patients if a beta-blocking agent is required. Beta blockers, including Lopressor HCT, may mask tachycardia occurring with hypoglycemia, but other manifestations such as dizziness and sweating may not be significantly affected. Selective beta blockers do not potentiate insulin-induced hypoglycemia and, unlike nonselective beta blockers, do not delay recovery of blood glucose to normal levels. Pheochromocytoma: If Lopressor is used in the setting of pheochromocytoma, it should be given in combination with an alpha blocker, and only after the alpha blocker has been initiated. Administration of beta blockers alone in the setting of pheochromocytoma has been associated with a paradoxical increase in blood pressure due to the attenuation of beta-mediated vasodilatation in skeletal muscle. Thyrotoxicosis: Beta-adrenergic blockade may mask certain clinical signs (e.g., tachycardia) or hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta blockade, which might precipitate a thyroid storm. HydrochlorothiazideThiazides should be used with caution in patients with severe renal disease. In patients with renal disease, thiazides may precipitate azotemia. Cumulative effects of the drug may develop in patients with impaired renal function. Thiazides should be used with caution in patients with impaired hepatic function or progressive liver disease, since minor alterations of fluid and electrolyte imbalance may precipitate hepatic coma. Thiazides may add to or potentiate the action of other antihypertensive drugs. Potentiation occurs with ganglionic or peripheral adrenergic blocking drugs. Sensitivity reactions are more likely to occur in patients with a history of allergy or bronchial asthma. The possibility of exacerbation or activation of systemic lupus erythematosus has been reported. PRECAUTIONSGeneralLopressor: Lopressor should be used with caution in patients with impaired hepatic function. Hydrochlorothiazide: All patients receiving thiazide therapy should be observed for clinical signs of fluid or electrolyte imbalance, namely hyponatremia, hypochloremic alkalosis, and hypokalemia (see Laboratory Tests and Drug/Drug Interactions). Warning signs are dryness of mouth, thirst, weakness, lethargy, drowsiness, restlessness, muscle pains or cramps, muscular fatigue, hypotension, oliguria, tachycardia, and gastrointestinal disturbance, such as nausea or vomiting. Hypokalemia may develop, especially in cases of brisk diuresis or severe cirrhosis. Interference with adequate oral intake of electrolytes will also contribute to hypokalemia. Hypokalemia may be avoided or treated by the use of potassium supplements or foods with high potassium content. Any chloride deficit is generally mild and usually does not require specific treatment, except under extraordinary circumstances (as in liver disease or renal disease). Dilutional hyponatremia may occur in edematous patients in hot weather; appropriate therapy is water restriction, rather than administration of salt, except in rare instances when the hyponatremia is life-threatening. In cases of actual salt depletion, appropriate replacement is the therapy of choice. Hyperuricemia may occur or frank gout may be precipitated in certain patients receiving thiazide therapy. Latent diabetes may become manifest during thiazide administration (see Drug/Drug Interactions). The antihypertensive effects of the drug may be enhanced in the postsympathectomy patient. If progressive renal impairment becomes evident, withholding or discontinuing diuretic therapy should be considered. Calcium excretion is decreased by thiazides. Pathological changes in the parathyroid gland with hypercalcemia and hypophosphatemia have been observed in a few patients on prolonged thiazide therapy. The common complications of hyperparathyroidism, such as renal lithiasis, bone resorption, and peptic ulceration, have not been seen. Thiazide diuretics have been shown to increase the urinary excretion of magnesium; this may result in hypomagnesemia. Information for PatientsPatients should be advised to take Lopressor HCT regularly and continuously, as directed, with or immediately following meals. If a dose should be missed, the patient should take only the next scheduled dose (without doubling it). Patients should not discontinue Lopressor HCT without consulting the physician. Patients should be advised (1) to avoid operating automobiles and machinery or engaging in other tasks requiring alertness until the patient’s response to therapy with Lopressor HCT has been determined; (2) to contact the physician if any difficulty in breathing occurs; (3) to inform the physician or dentist before any type of surgery that he or she is taking Lopressor HCT. Laboratory TestsLopressor: Clinical laboratory findings may include elevated levels of serum transaminase, alkaline phosphatase, and lactate dehydrogenase. Hydrochlorothiazide: Initial and periodic determinations of serum electrolytes to detect possible electrolyte imbalance should be performed at appropriate intervals. Serum and urine electrolyte determinations are particularly important when the patient is vomiting excessively or receiving parenteral fluids. Drug/Drug InteractionsLopressor: Catecholamine-depleting drugs (e.g., reserpine) may have an additive effect when given with beta-blocking agents. Patients treated with Lopressor plus a catecholamine depletor should therefore be closely observed for evidence of hypotension or marked bradycardia, which may produce vertigo, syncope, or postural hypotension. Both digitalis glycosides and beta blockers slow atrioventricular conduction and decrease heart rate. Concomitant use can increase the risk of bradycardia. Risk of Anaphylactic Reaction: While taking beta blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction. General AnestheticsSome inhalation anesthetics may enhance the cardiodepressant effect of beta blockers (see WARNINGS; Lopressor; Major Surgery). CYP2D6 InhibitorsPotent inhibitors of the CYP2D6 enzyme may increase the plasma concentration of Lopressor. Strong inhibition of CYP2D6 would mimic the pharmacokinetics of CYP2D6 poor metabolizer. Caution should therefore be exercised when administering potent CYP2D6 inhibitors with Lopressor. Known clinically significant potent inhibitors of CYP2D6 are antidepressants such as fluoxetine, paroxetine or bupropion, antipsychotics such as thioridazine, antiarrhythmics such as quinidine or propafenone, antiretrovirals such as ritonavir, antihistamines such as diphenhydramine, antimalarials such as hydroxychloroquine or quinidine, antifungals such as terbinafine and medications for stomach ulcers such as cimetidine. ClonidineIf a patient is treated with clonidine and Lopressor concurrently, and clonidine treatment is to be discontinued, Lopressor should be stopped several days before clonidine is withdrawn. Rebound hypertension that can follow withdrawal of clonidine may be increased in patients receiving concurrent beta blocker treatment. Hydrochlorothiazide: Hypokalemia can sensitize or exaggerate the response of the heart to the toxic effects of digitalis (e.g., increased ventricular irritability). Hypokalemia may develop during concomitant use of steroids or ACTH. Insulin requirements in diabetic patients may be increased, decreased, or unchanged. Thiazides may decrease arterial responsiveness to norepinephrine, but not enough to preclude effectiveness of the pressor agent for therapeutic use. Thiazides may increase the responsiveness to tubocurarine. Lithium renal clearance is reduced by thiazides, increasing the risk of lithium toxicity. There have been rare reports in the literature of hemolytic anemia occurring with the concomitant use of hydrochlorothiazide and methyldopa. Concurrent administration of some nonsteroidal anti-inflammatory agents may reduce the diuretic, natriuretic and antihypertensive effects of thiazide diuretics. Cholestyramine and colestipol resins: Absorption of hydrochlorothiazide is impaired in the presence of anionic exchange resins. Single doses of either cholestyramine or colestipol resins bind the hydrochlorothiazide and reduce its absorption from the gastrointestinal tract by up to 85% and 43%, respectively. Drug/Laboratory Test InteractionsHydrochlorothiazide: Thiazides may decrease serum levels of protein-bound iodine without signs of thyroid disturbance. Thiazides should be discontinued before tests for parathyroid function are made. (see General, Hydrochlorothiazide, Calcium excretion). Carcinogenesis, Mutagenesis, Impairment of FertilityLopressor HCT: Carcinogenicity and mutagenicity studies have not been conducted with Lopressor HCT. Lopressor HCT produced no evidence of impaired fertility in male or female rats administered gavaged doses up to 200/50 mg/kg (100/50 times the maximum recommended daily human dose) prior to mating and throughout gestation and rearing of young. Lopressor: Long-term studies in animals have been conducted to evaluate carcinogenic potential. In a 2-year study in rats at three oral dosage levels of up to 800 mg/kg per day, there was no increase in the development of spontaneously occurring benign or malignant neoplasms of any type. The only histologic changes that appeared to be drug related were an increased incidence of generally mild focal accumulation of foamy macrophages in pulmonary alveoli and a slight increase in biliary hyperplasia. In a 21-month study in Swiss albino mice at three oral dosage levels of up to 750 mg/kg per day, benign lung tumors (small adenomas) occurred more frequently in female mice receiving the highest dose than in untreated control animals. There was no increase in malignant or total (benign plus malignant) lung tumors, or in the overall incidence of tumors or malignant tumors. This 21-month study was repeated in CD-1 mice, and no statistically or biologically significant differences were observed between treated and control mice of either sex for any type of tumor. All mutagenicity tests performed (a dominant lethal study in mice, chromosome studies in somatic cells, a Salmonella/mammalian-microsome mutagenicity test, and a nucleus anomaly test in somatic interphase nuclei) were negative. No evidence of impaired fertility due to Lopressor was observed in a study performed in rats at doses up to 55.5 times the maximum daily human dose of 450 mg. Hydrochlorothiazide: Two-year feeding studies in mice and rats conducted under the auspices of the National Toxicology Program (NTP) uncovered no evidence of a carcinogenic potential of hydrochlorothiazide in female mice (at doses up to approximately 600 mg/kg/day) or in male and female rats (at doses up to approximately 100 mg/kg/day). The NTP, however, found equivocal evidence for hepatocarcinogenicity in male mice. Hydrochlorothiazide was not genotoxic in in vitro assays using strains TA 98, TA 100, TA 1535, TA 1537, and TA 1538 of Salmonella typhimurium (Ames assay) and in the Chinese Hamster Ovary (CHO) test for chromosomal aberrations, or in in vivo assays using mouse germinal cell chromosomes, Chinese hamster bone marrow chromosomes, and the Drosophila sex-linked recessive lethal trait gene. Positive test results were obtained only in the in vitro CHO Sister Chromatid Exchange (clastogenicity) and in the Mouse Lymphoma Cell (mutagenicity) assays, using concentrations of hydrochlorothiazide from 43 to 1300 µg/mL, and in the Aspergillus nidulans nondisjunction assay at an unspecified concentration. Hydrochlorothiazide had no adverse effects on the fertility of mice and rats of either sex in studies wherein these species were exposed, via their diet, to doses of up to 100 and 4 mg/kg/day, respectively, prior to mating and throughout gestation. Pregnancy: Teratogenic Effects. Pregnancy Category CLopressor HCT: No evidence of adverse effects on pregnancy or the fetus were observed in rats when dams were administered gavaged doses up to 200/50 mg/kg of Lopressor HCT (100/50 times the maximum recommended daily human dose) during the period of organogenesis. Increased postimplantation loss and decreased postnatal survival were observed with these doses when administered later in pregnancy (gestation days 15-21). In rabbits, increased fetal loss was observed with oral doses of 25/6.25 mg/kg of Lopressor HCT (12/6 times the maximum recommended daily human dose), but not with lower doses. There are no adequate and well-controlled studies of Lopressor HCT in pregnant women. Lopressor HCT should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Lopressor: Lopressor has been shown to increase postimplantation loss and decrease neonatal survival in rats at doses up to 55.5 times the maximum daily human dose of 450 mg. Distribution studies in mice confirm exposure of the fetus when Lopressor is administered to the pregnant animal. These studies have revealed no evidence of teratogenicity. Hydrochlorothiazide: Studies in which hydrochlorothiazide was orally administered to pregnant mice and rats during their respective periods of major organogenesis at doses up to 3000 and 1000 mg/kg/day, respectively, provided no evidence of harm to the fetus. Nonteratogenic EffectsHydrochlorothiazide: Thiazides cross the placental barrier and appear in cord blood, and there is a risk of fetal or neonatal jaundice, thrombocytopenia, and possibly other adverse reactions that have occurred in adults. Nursing MothersLopressor is excreted in breast milk in a very small quantity. An infant consuming 1 liter of breast milk daily would receive a dose of metoprolol of less than 1 mg. Thiazides are also excreted in breast milk. If the use of Lopressor HCT is deemed essential, the patient should stop nursing. Pediatric UseSafety and effectiveness in pediatric patients have not been established. Geriatric UseClinical studies of Lopressor HCT did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. Hydrochlorothiazide is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function (see WARNINGS). In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and concomitant disease or other drug therapy. ADVERSE REACTIONSLopressor HCTThe following adverse reactions were reported in controlled clinical studies of the combination of Lopressor and hydrochlorothiazide. Body as a Whole: Fatigue or lethargy and flu syndrome have each been reported in about 10 in 100 patients. Nervous System: Dizziness or vertigo, drowsiness or somnolence, and headache have each occurred in about 10 in 100 patients. Nightmare has occurred in 1 in 100 patients. Cardiovascular: Bradycardia has occurred in about 6 in 100 patients. Decreased exercise tolerance and dyspnea have each occurred in about 1 of 100 patients. Digestive: Diarrhea, digestive disorder, dry mouth, nausea or vomiting, and constipation have each occurred in about 1 in 100 patients. Metabolic and Nutritional: Hypokalemia has occurred in fewer than 10 in 100 patients. Edema, gout, and anorexia have each occurred in 1 in 100 patients. Special Senses: Blurred vision, tinnitus, and earache have each been reported in 1 in 100 patients. Skin: Sweating and purpura have each occurred in 1 in 100 patients. Urogenital: Impotence has occurred in 1 in 100 patients. Musculoskeletal: Muscle pain has occurred in 1 in 100 patients. LopressorMost adverse effects have been mild and transient. Central Nervous System: Tiredness and dizziness have occurred in about 10 of 100 patients. Depression has been reported in about 5 of 100 patients. Mental confusion and short-term memory loss have been reported. Headache, nightmares, and insomnia have also been reported, but a drug relationship is not clear. Cardiovascular: Shortness of breath and bradycardia have occurred in approximately 3 of 100 patients. Cold extremities; arterial insufficiency, usually of the Raynaud type; palpitations; and congestive heart failure have been reported. Gangrene in patients with pre-existing severe peripheral circulatory disorders has also been reported very rarely (see CONTRAINDICATIONS, WARNINGS, and PRECAUTIONS). Respiratory: Wheezing (bronchospasm) has been reported in fewer than 1 of 100 patients (see WARNINGS). Rhinitis has also been reported. Gastrointestinal: Diarrhea has occurred in about 5 of 100 patients. Nausea, gastric pain, constipation, flatulence, and heartburn have been reported in 1 of 100, or fewer, patients. Vomiting was a common occurrence. Postmarketing experience reveals very rare reports of hepatitis, jaundice and non-specific hepatic dysfunction. Isolated cases of transaminase, alkaline phosphatase, and lactic dehydrogenase elevations have also been reported. Hypersensitive Reactions: Pruritus has occurred in fewer than 1 of 100 patients. Rash has been reported. Very rarely, photosensitivity and worsening of psoriasis has been reported. Miscellaneous: Peyronie’s disease has been reported in fewer than 1 of 100,000 patients. Alopecia has been reported. There have been very rare reports of weight gain, arthritis, and retroperitoneal fibrosis (relationship to Lopressor has not been definitely established). The oculomucocutaneous syndrome associated with the beta blocker practolol has not been reported with Lopressor. Potential Adverse ReactionsA variety of adverse reactions not listed above have been reported with other beta-adrenergic blocking agents and should be considered potential adverse reactions to Lopressor. Central Nervous System: Reversible mental depression progressing to catatonia; visual disturbances; hallucinations; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, slightly clouded sensorium, and decreased performance on neuropsychometrics. Cardiovascular: Intensification of AV block (see CONTRAINDICATIONS). Hematologic: Agranulocytosis, nonthrombocytopenic purpura, thrombocytopenic purpura. Hypersensitive Reactions: Fever combined with aching and sore throat, laryngospasm, and respiratory distress. Postmarketing ExperienceThe following adverse reactions have been reported during postapproval use of Lopressor: confusional state, an increase in blood triglycerides and a decrease in High Density Lipoprotein (HDL). Because these reports are from a population of uncertain size and are subject to confounding factors, it is not possible to reliably estimate their frequency. HydrochlorothiazideThe following adverse reactions have been observed, but there has not been enough systematic collection of data to support an estimate of their frequency. Consequently the reactions are categorized by organ systems and are listed in decreasing order of severity and not frequency. Digestive: Pancreatitis, jaundice (intrahepatic cholestatic), sialadenitis, vomiting, diarrhea, cramping, nausea, gastric irritation, constipation, anorexia. Cardiovascular: Orthostatic hypotension (may be potentiated by alcohol, barbiturates, or narcotics). Neurologic: Vertigo, dizziness, transient blurred vision, headache, paresthesia, xanthopsia, weakness, restlessness. Musculoskeletal: Muscle spasm. Hematologic: Aplastic anemia, agranulocytosis, leukopenia, thrombocytopenia. Metabolic: Hyperglycemia, glycosuria, hyperuricemia. Hypersensitive Reactions: Necrotizing angiitis, Stevens-Johnson syndrome, respiratory distress including pneumonitis and pulmonary edema, purpura, urticaria, rash, photosensitivity. OVERDOSAGEAcute ToxicitySeveral cases of overdosage with Lopressor have been reported, some leading to death. No deaths have been reported with hydrochlorothiazide. Oral LD 50’s (mg/kg): mice, 1158 (Lopressor); rats, 3090 (Lopressor), 2750 (hydrochlorothiazide). Signs and SymptomsLopressor: Potential signs and symptoms associated with overdosage with Lopressor are bradycardia, hypotension, bronchospasm, and cardiac failure. Hydrochlorothiazide: The most prominent feature of poisoning is acute loss of fluid and electrolytes. Cardiovascular: Tachycardia, hypotension, shock. Neuromuscular: Weakness, confusion, dizziness, cramps of the calf muscles, paresthesia, fatigue, impairment of consciousness. Digestive: Nausea, vomiting, thirst. Renal: Polyuria, oliguria, or anuria (due to hemoconcentration). Laboratory Findings: Hypokalemia, hyponatremia, hypochloremia, alkalosis; increased BUN (especially in patients with renal insufficiency). Combined Poisoning: Signs and symptoms may be aggravated or modified by concomitant intake of antihypertensive medication, barbiturates, curare, digitalis (hypokalemia), corticosteroids, narcotics, or alcohol. TreatmentThere is no specific antidote. On the basis of the pharmacologic actions of Lopressor and hydrochlorothiazide, the following general measures should be employed: Elimination of the Drug: Inducement of vomiting, gastric lavage, and activated charcoal. Bradycardia: Atropine should be administered. If there is no response to vagal blockade, isoproterenol should be administered cautiously. Hypotension: The patient’s legs should be elevated and lost fluid and electrolytes (potassium, sodium) should be replaced. A vasopressor should be administered, e.g., levarterenol or dopamine. Bronchospasm: A beta2-stimulating agent and/or a theophylline derivative should be administered. Cardiac Failure: A digitalis glycoside and diuretic should be administered. In shock resulting from inadequate cardiac contractility, administration of dobutamine, isoproterenol, or glucagon may be considered. Surveillance: Fluid and electrolyte balance (especially serum potassium) and renal function should be monitored until conditions become normal. DOSAGE AND ADMINISTRATIONDosage should be determined by individual titration (see INDICATIONS AND USAGE). Hydrochlorothiazide is usually given at a dosage of 12.5 to 50 mg per day. The usual initial dosage of Lopressor is 100 mg daily in single or divided doses. Dosage may be increased gradually until optimum blood pressure control is achieved. The effective dosage range is 100 to 450 mg per day. While once-daily dosing is effective and can maintain a reduction in blood pressure throughout the day, lower doses (especially 100 mg) may not maintain a full effect at the end of the 24-hour period, and larger or more frequent daily doses may be required. This can be evaluated by measuring blood pressure near the end of the dosing interval to determine whether satisfactory control is being maintained throughout the day. Beta1 selectivity diminishes as dosage of Lopressor is increased. The following dosage schedule may be used to administer from 100 to 200 mg of Lopressor per day and from 25 to 50 mg of hydrochlorothiazide per day:
Dosing regimens that exceed 50 mg of hydrochlorothiazide per day are not recommended. When necessary, another antihypertensive agent may be added gradually, beginning with 50% of the usual recommended starting dose to avoid an excessive fall in blood pressure. HOW SUPPLIEDTablets 50/25 - capsule-shaped, white and mottled-blue, scored (imprinted Geigy on one side and 35 twice on the scored side), 50 mg of metoprolol tartrate and 25 mg of hydrochlorothiazide Bottles of 100……………………………………NDC 0078-0460-05 Tablets 100/25 - capsule-shaped, white and mottled-pink, scored (imprinted Geigy on one side and 53 twice on the scored side), 100 mg of metoprolol tartrate and 25 mg of hydrochlorothiazide Bottles of 100……………………………………NDC 0078-0461-05 Tablets 100/50 - capsule- shaped, white and mottled-yellow, scored (imprinted Geigy on one side and 73 twice on the scored side), 100 mg of metoprolol tartrate and 50 mg of hydrochlorothiazide Bottles of 100……………………………………NDC 0078-0462-05 Store at 25ºC (77ºF); excursions permitted to 15-30ºC (59-86ºF) [see USP Controlled Room Temperature]. Protect from moisture. Dispense in tight, light-resistant container (USP). |
LOPRESSOR HCT(酒石酸美托洛尔/氢氯噻嗪片)简介:
【药物名称】中文通用名称:酒石酸美托洛尔英文通用名称:Metoprolol Tartrate其它名称:倍他乐克、伯他乐安、甲氧乙心安、酒石酸美多心安、美多洛尔、美多心安、美他新、美托洛尔、蒙得康、素可丁、托西 ... 责任编辑:admin |
最新文章更多推荐文章更多热点文章更多
|