|
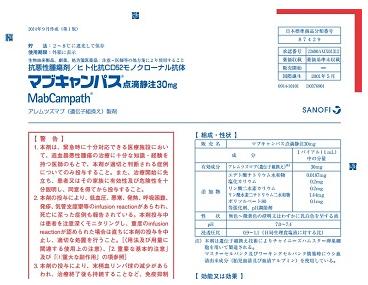
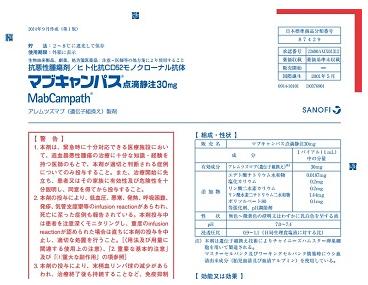
英文药名:MabCampath(Alemtuzumab[Genetical Recombination])
中文药名:阿仑单抗重组注射剂
生产厂家:赛诺菲公司
マブキャンパス点滴静注30mg
药物分类名称
抗肿瘤药/人源化抗CD52单克隆抗体
批准日期:2015年1月
商標名
MabCampath
一般名
アレムツズマブ(遺伝子組換え)
Alemtuzumab(Genetical Recombination)
本質
阿仑单抗是重组人源化单克隆抗体,由大鼠抗人CD52抗体的互补决定部分构成,构架部分和人IgG1的常数部分组成。 阿美珠珠单抗是由中国仓鼠卵巢细胞产生的。 阿列珠单抗是由由214个氨基酸残基组成的2分子的L链(κ链)和由450个氨基酸残基组成的2个H链(γ1链)组成的糖蛋白(分子量约为15万)。
批准条件
由于日本的临床试验数量非常有限,通过对所有病例进行使用情况调查,直到制作销售后累积了一定数量的病例, 除了掌握使用患者的背景资料外,尽快收集有关该药物安全性和有效性的资料,并采取必要措施,妥善使用该药。
药效药理
该药物是与CD52抗原结合的人源化单克隆抗体。 CD52抗原在B细胞,T细胞,单核细胞,巨噬细胞,天然杀伤细胞和慢性淋巴细胞白血病(CLL)细胞中表达。 据认为,该药物与慢性淋巴细胞性白血病细胞表面的CD52抗原结合,通过抗体依赖性细胞毒性(ADCC)活性和补体依赖性细胞毒性(CDC)活性诱导细胞裂解。
适应病症
复发性或难治性慢性淋巴细胞性白血病
用法与用量
成年人,静脉滴注3mg,每天一次,静脉滴注10mg,每天一次,每天一次,每天三次,每次三次,每次三次,间隔天数 静脉滴注 但是,从管理开始,管理应该长达12周。 此外,根据患者的状况进行体重减轻。
存储方式·到期日等
保存方法
存放于2-8°C,避光
包装规格
30毫克(1毫升)×1瓶

制造和销售
日本赛诺菲公司
注:以上中文资料不够完整,使用以原处方为准
完整资料附件:http://www.info.pmda.go.jp/go/pack/4291428A1029_1_03/
MABCAMPATH
Solution for intravenous infusion
COMPOSITION
Each ampoule contains 30 mg alemtuzumab (10mg/mL concentrate solution).
PHARMACOLOGICAL CLASSIFICATION
A. 26 Cytostatic agents.
PHARMACOLOGICAL ACTION
Pharmacodynamic properties
Alemtuzumab is a genetically engineered humanised IgG1 kappa monoclonal antibody specific for a 21 to 28 kD lymphocyte cell surface glycoprotein (CD52) expressed primarily on the surface of normal and malignant peripheral blood B and T cell lymphocytes. Alemtuzumab was generated by the insertion of six complementarity-determining regions from an IgG2a rat monoclonal antibody into a human IgG1 immunoglobulin molecule.
Alemtuzumab causes the lysis of lymphocytes by binding to CD52, a highly expressed, non-modulating antigen which is present on the surface of essentially all B and T cell lymphocytes as well as monocytes, thymocytes and macrophages. The antigen has also been found on a small percentage (<5%) of granulocytes, but not on erythrocytes or platelets. The antibody mediates the lysis of lymphocytes via complement fixation and antibody-dependent cell mediated cytotoxicity. Alemtuzumab does not appear to damage haematopoietic stem cells or progenitor cells.
Pharmacokinetic properties
The pharmacokinetics of alemtuzumab were studied in patients who received MabCampath once weekly for a maximum of 12 weeks. Following single intravenous infusions of 7,5 mg, 24 mg or 75 mg, the maximum serum concentration (Cmax) and the area under the curve (AUC) showed relative dose proportionality. The median half-life ranged from ~ 23 to 30 hours.
The pharmacokinetics and pharmacodynamics profile of MabCampath administered as a 30 mg intravenous infusion 3 times per week was evaluated in non-Hodgkin’s lymphoma and chronic lymphocytic leukaemia patients who were treated for a maximum of 12 weeks. In patients with chronic lymphocytic leukaemia, peak and trough levels of MabCampath rose during the first few weeks of treatment and then approached steady state by approximately week 6. The rise in serum concentration corresponded with a marked reduction in lymphocytosis. Patients with peripheral lymphocyte counts of >30 000/microL at baseline had significantly lower peak and trough levels of MabCampath during the first 4 to 5 weeks of treatment compared to those with lymphocyte counts <30 000 microL. This suggests that lymphocytosis represents a compartment in the blood in which MabCampath is concentrated.
INDICATIONS
MabCampath is indicated for the treatment of patients with chronic lymphocytic leukaemia who have been treated with alkylating agents and who have failed to achieve a complete or partial response or who achieved only a short remission (less than 6 months) following fludarabine phosphate therapy.
CONTRA-INDICATIONS
• Tuberculosis and latent tuberculosis.
• Patients exposed to people with tuberculosis (TB).
• Patients exposed to patients recently immunised with live attenuated vaccines.
• Hypersensitivity or anaphylactic reactions to alemtuzumab, to murine proteins, or to any of the excipients.
• In patients with active systemic infections.
• In patients infected with HIV.
• In patients with active secondary malignancies.
• Pregnancy and breast-feeding, as safety and efficacy have not been demonstrated.
• In children as safety and efficacy is not established.
• In patients with renal and hepatic impairment (see “Dosage and directions for use”).
WARNINGS
Acute adverse reactions may occur during initial dose escalation due to the release of cytokines and include hypotension, rigors, fever, shortness of breath, chills and rashes. If these events are moderate to severe, then dosing should continue at the same level with appropriate premedication, until each dose is well tolerated (eg infusion-related toxicities are <grade 2). See “Dosage and directions for use” for dose adjustments and/or discontinuation of treatment. If therapy is withheld for more than 7 days, MabCampath should be reinstituted with gradual dose escalation.
Transient hypotension has occurred in patients receiving MabCampath. Caution should be used in treating patients with ischaemic heart disease, angina and/or in patients receiving antihypertensive medication.
It is recommended that patients be premedicated with an oral antihistamine and an analgesic 30 minutes prior to first MabCampath treatment at 3 mg, at each subsequent dose escalation, and thereafter, if clinically indicated. The recommended premedication is per oral 50 mg diphenhydramine and 500 mg paracetamol. In cases where severe infusion-related events prevent escalation of the dose, pre-treatment with intravenous (iv) 200 mg hydrocortisone may be useful in decreasing infusion-related reactions.
Profound lymphocyte depletion inevitably occurs and may be prolonged. CD4 and CD8 lymphocyte counts begin to rise following the discontinuation of treatment, but may not return to baseline levels for periods of longer than a year. This may predispose patients to opportunistic infections such as tuberculosis, acute bacterial pneumonia and septicaemia. It is highly recommended that anti-infective prophylaxis against Pneumocystis carinii pneumonia and an oral anti-herpes agent should be initiated while on therapy, and administered up to a minimum of 2 months following cessation of MabCampath treatment. If severe or serious infection does occur, MabCampath treatment should be discontinued until the event has resolved. MabCampath treatment may be reinstituted following resolution of the event.
Grade 3 or 4 neutropenia occurs very commonly by weeks 5 to 8 following initiation of treatment. Grade 3 or 4 thrombocytopenia occurs very commonly during the first 2 weeks of therapy and then begins to improve in most patients. Therefore, close haematological monitoring of patients is indicated. If severe haematological toxicity develops, MabCampath treatment should be discontinued until the event resolves. MabCampath treatment may be reinstituted following resolution of the haematological toxicity (see “Dosage and directions for use”).
Complete blood counts and platelet counts should be obtained at regular intervals during MabCampath therapy, and more frequently in patients who develop cytopenias.
It is not proposed that regular and systematic monitoring of CD52 expression should be carried out as routine clinical practice. However, if retreatment is considered, it may be prudent to confirm the presence of CD52 expression.
Patients may have allergic or hypersensitivity reactions to MabCampath and to murine or chimeric monoclonal antibodies.
Males and females of childbearing potential should use effective contraceptive measures during treatment and for 6 months following MabCampath therapy.
No studies have been conducted which specifically address the effect of age on MabCampath disposition and toxicity. In general, older patients (over 65 years of age) tolerate cytotoxic therapy less well than younger individuals. Since chronic lymphocytic leukaemia occurs commonly in this older age group, these patients should be monitored carefully (see “Dosage and directions for use”).
INTERACTIONS
No formal drug interaction studies have been performed with MabCampath. There are no known clinically significant interactions of MabCampath with other medicinal products. However, it is recommended that MabCampath should not be given within 3 weeks of other chemotherapeutic agents.
Although it has not been studied, it is recommended that patients should not receive live viral vaccines in, at least, the 12 months following MabCampath therapy. The ability to generate a primary or anamnestic humoral response to any vaccine has not been studied.
PREGNANCY AND LACTATION
See “Contra-indications”.
DOSAGE AND DIRECTIONS FOR USE
MabCampath should be administered under the supervision of a physician experienced in the use of cancer therapy.
Patients should be premedicated with an appropriate antihistamine and analgesic prior to the first dose, at each escalation, and prior to subsequent infusions, as clinically indicated (see “Warnings”).
Antibiotics and antivirals should be administered routinely to all patients throughout and following treatment (see “Warnings”).
During the first week of treatment, MabCampath should be administered in escalating doses: 3 mg on day 1, 10 mg on day 2 and 30 mg on day 3, assuming that each dose is well tolerated (eg infusion-related toxicities are < grade 2). Thereafter, the recommended dose is 30 mg daily administered 3 times weekly on alternate days, up to a maximum of 12 weeks.
In most patients, dose escalation to 30 mg can be accomplished in 3 to 7 days. However, if acute severe adverse reactions (especially hypotension, rigors, fever and bronchospasm) occur at either the 3 mg or 10 mg dose levels, then those doses should be repeated daily until they are well tolerated prior to further escalation (see “Warnings”).
The majority of major responses to MabCampath have been achieved with treatment durations of 4 to 12 weeks. Once a patient meets all laboratory and clinical criteria for a complete response, MabCampath should be discontinued and the patient monitored. If a patient improves (ie achieves a partial response or stable disease) and then reaches a plateau without further improvement for 4 weeks or more, then MabCampath should be discontinued and the patient monitored. Therapy should be discontinued if there is evidence of disease progression.
In the event of serious infection or severe haematological toxicity, MabCampath should be discontinued until the event resolves. It is recommended that MabCampath should be discontinued in patients whose platelet count fills to <25 000/microL or whose absolute neutrophil count (ANC) drops to <250/microL. MabCampath may be reinstituted after the infection or toxicity has resolved. The following table outlines the recommended procedure for dose modification following the occurrence of haematological toxicity while on therapy:
Haematological toxicity
(platelets <25 000/ microL and/or ANC <250/microL) |
Reinstitution of MabCampath |
| First occurrence |
After resolution, reinstitute at 30 mg * |
| Second occurrence |
After resolution, reinstitute at 10 mg * |
| Third occurrence |
Permanent discontinuation | * If therapy has been withheld for more than 7 days, MabCampath must be reinstituted by gradual dose escalation.
Children and adolescents (below 17 years of age):
No studies have been conducted (see “Contra-indications”).
Elderly (over 65 years of age):
Recommendations are as stated above for adults. Patients should be monitored carefully (see “Warnings”).
Patients with renal or hepatic impairment:
Treatment with MabCampath is not recommended (see “Warnings”).
All doses should be administered by intravenous infusion over approximately 2 hours.
The ampoule contents should be inspected for particulate matter and discolouration prior to administration. If particulate matter is present or the concentrate is coloured, then the ampoule should not be used.
MabCampath contains no antimicrobial preservatives, therefore it is recommended that it should be prepared using aseptic techniques and that the diluted solution for infusion should be administered immediately or within 8 hours after preparation. The required amount of the ampoule contents should be added, via a sterile, low-protein binding, non-fibre 5 micron filter, to 100 mL of 0,9% sodium chloride solution or 5% glucose solution. The bag should be inverted gently to mix the solution.
This medicinal product should not be reconstituted with solvents other than sodium chloride and glucose solution.
There are no known incompatibilities with other medicinal products.
Other medicinal products should not be added to the MabCampath infusion solution or simultaneously infused through the same intravenous line.
Women who are pregnant or planning pregnancy should not handle MabCampath.
Procedures for proper handling and disposal should be observed. Any spillage or waste material should be disposed of by incineration.
Caution should be exercised in the handling and preparation of the MabCampath solution. The use of latex gloves and safety glasses is recommended to avoid exposure in case of breakage of the ampoule or other accidental spillage.
SIDE EFFECTS AND SPECIAL PRECAUTIONS
More than 80% of patients may be expected to experience adverse reactions; the most commonly reported reactions usually occurring during the first week of therapy.
Infusion-related reactions
Reactions reported have been acute infusion-related reactions including fever, rigors, nausea, vomiting, hypotension, fatigue, rash, urticaria, dyspnoea, headache, pruritus and diarrhoea. The majority of these reactions are mild to moderate in severity. Acute infusion-related reactions usually occur during the first week of therapy and decline substantially thereafter. Grade 3 or 4 infusion-related reactions are uncommon after the first week of therapy. These symptoms can be ameliorated or avoided if premedication and dose escalation are utilised (see “Warnings”).
Infections
Grade 3 or 4 infections have been reported, including herpes simplex and pneumonia of grade 3 or 4 severity. Opportunistic infections including Pneumocystis carinii pneumonia, cytomegalovirus, Aspergillus pneumonia and herpes zoster occur. Rhinocerebral mucormycosis has been reported. None of the patients with Pneumocystis carinii pneumonia or herpes zoster had received the anti-infective prophylaxis. Such therapy appears to be effective in reducing the risk of infections due to these opportunistic pathogens (see “Warnings”).
Haematological reactions
Severe bleeding reactions have been reported. One patient developed fatal idiopathic thrombocytopenic purpura following MabCampath therapy. Pancytopenia has been reported and may be grade 3 or 4 in severity or serious in nature. A positive Coombs test is observed; clinically apparent haemolysis has not been reported in patients treated to date.
The table below reports adverse reactions by body system and in descending order of severity:
| Body system |
Adverse reactions and infections |
| |
Very common
(>10%) |
Common
(>1% to 10%) |
Uncommon
(>0,1% to 1%) |
| Application site |
|
Injection site reaction |
Injection site bruising
Injection site dermatitis
Injection site pain |
| Body as a whole –general |
Rigors
Fever
Fatigue
Anorexia |
Back pain
Neutropenic fever
Chest pain
Pain
Oedema mouth
Asthenia
Malaise
Influenza-like symptoms
Oedema
Temperature change sensation |
Syncope
Oedema peripheral
Leg pain
Allergic reaction |
| Cardiovascular |
Hypotension |
Hypertension
Tachycardia
Vasospasm
Flushing
Palpitation |
Cardiac arrest
Myocardial infarction
Fibrillation atrial
Tachycardia
supraventricular
ECG abnormal
Arrhythmia
Bradycardia
Peripheral ischaemia |
| Central and peripheral nervous including vision, hearing and special senses |
Headache |
Taste loss
Tremor
Hypoaesthesia
Dizziness
Hyperkinesia
Conjunctivitis
Paraesthesia
Vertigo |
Gait abnormal
Endophthalmitis
Dystonia
Hyperaesthesia
Hypertonia
Deafness
Tinnitus
Taste perversion
Neuropathy |
| Gastro-intestinal, liver and biliary |
Vomiting
Nausea
Diarrhoea |
Abdominal pain
Gastro-intestinal
haemorrhage
Stomatitis
Mucositis
Hepatic function abnormal
Constipation
Dyspepsia
Stomatitis ulcerative
Flatulence |
Gastroenteritis
Gingivitis
Eructation
Hiccup
Mouth dry
Mucosal ulceration
Tongue ulceration |
| Haematological |
|
Granulocytopenia
Thrombocytopenia
Anaemia
Pancytopenia
Leukopenia
Lymphopenia
Purpura |
Aplasia bone marrow
Haptoglobin decreased
Disseminate intravascular
coagulation
Anaemia haemolytic
Marrow depression
Epistaxis
Gingival bleeding
Haematology value
Abnormal |
| Metabolic and nutritional |
|
Hyponatraemia
Dehydration
Weight decrease
Hypocalcaemia
Thirst |
Diabetes mellitus
aggravated
Oedema periorbital
Hypokalaemia |
| Musculo-skeletal |
|
Skeletal pain
Arthralgia
Myalgia |
|
| Neoplasm |
|
|
Lymphoma-like disorder |
| Psychiatric |
|
Confusion
Anxiety
Somnolence
Depression
Insomnia |
Nervousness
Thinking abnormal
Depersonalisation
Impotence
Personality disorder |
| Resistance mechanism |
Sepsis
Herpes simplex |
Cytomegalovirus infection
Pneumocystis carinii
infection
Moniliasis
Herpes zoster
Infection
Infection fungal
Abscess |
Infection viral
Infection bacterial |
| Respiratory |
Pneumonia
Dyspnoea |
Pneumonitis
Bronchospasm
Sinusitis
Coughing
Hypoxia
Upper tract infection
Bronchitis
Pharyngitis
Haemoptysis |
Pulmonary oedema
Stridor
Pulmonary infiltration
Respiratory disorder
Breath sounds decreased
Laryngitis
Rhinitis
Throat tightness
Pleural effusion |
| Skin and appendages |
Urticaria
Rash
Pruritus
Sweating increased |
Rash erythematous
Bullous eruption |
Dermatitis fungal
Onychomycosis
Rash maculo-papular
Skin disorder |
| Urinary |
|
Urinary tract infection |
Renal function abnormal
Polyuria
Haematuria
Urinary incontinence
Urine flow decreased. | KNOWN SYMPTOMS OF OVERDOSAGE AND PARTICULARS OF ITS TREATMENT
Patients have received repeated unit doses of up to 240 mg of MabCampath. The frequency of grade 3 or 4 adverse events such as fever, hypotension and anaemia may be higher in these patients. There is no known specific antidote for MabCampath overdosage. Treatment consists of discontinuation of MabCampath and supportive therapy.
IDENTIFICATION
Clear, colourless to slightly yellow solution, essentially free from visible particles.
PRESENTATION
Each cardboard carton contains 3x5mL clear glass ampoules each with 3 mL concentrate.
STORAGE INSTRUCTIONS
Store at 2 to 8°C in a refrigerator. Do not freeze. Protect from light. Do not remove from the outer container until immediately before use. Keep out of reach of children. Discard any unused portion of the solution.
Reconstituted solution
MabCampath contains no antimicrobial preservative. MabCampath should be used immediately after dilution or within 8 hours if stored at 15 to 30°C. This can only be accepted if preparation of the solution takes place under strict aseptic conditions and the solution is protected from light. |