Exjade Dosage and Administration
Dosing Information
Prior to starting therapy, obtain baseline serum ferritin and iron levels. The risk for toxicity may be increased when Exjade is given to patients with low iron burden or with serum ferritin levels that are only slightly elevated [see Dose Modifications (2.2)].
The recommended initial daily dose of Exjade is 20 mg/kg body weight.
Take Exjade once daily on an empty stomach at least 30 minutes before food, preferably at the same time each day. Do not chew tablets or swallow them whole. Do not take Exjade with aluminum-containing antacid products. Calculate doses (mg/kg per day) to the nearest whole tablet. Completely disperse tablets by stirring in water, orange juice, or apple juice until a fine suspension is obtained. Disperse doses of <1 g in 3.5 ounces of liquid and doses of ≥1 g in 7.0 ounces of liquid. After swallowing the suspension, resuspend any residue in a small volume of liquid and swallow.
Individualize the decision to remove accumulated iron based on anticipated clinical benefit and risks of Exjade therapy. In patients who are in need of iron chelation therapy, it is recommended that therapy with Exjade (deferasirox) be started when a patient has evidence of chronic iron overload, such as the transfusion of approximately 100 mL/kg of packed red blood cells (approximately 20 units for a 40-kg patient) and a serum ferritin consistently >1000 mcg/L.
Dose Modifications
Exjade may require dose adjustment, interruption or cessation of the therapy due to toxicity or any of the following [see Warnings and Precautions (5.1-5.6), Geriatric Use (8.5)]:
Based on Serum Ferritin
After commencing initial therapy, monitor serum ferritin every month and adjust the dose of Exjade if necessary every 3-6 months based on serum ferritin trends. Make dose adjustments in steps of 5 or 10 mg/kg and tailor adjustments to the individual patient’s response and therapeutic goals (maintenance or reduction of body iron burden). In patients not adequately controlled with doses of 30 mg/kg (e.g., serum ferritin levels persistently above 2500 mcg/L and not showing a decreasing trend over time), doses of up to 40 mg/kg may be considered. Doses above 40 mg/kg are not recommended.
If the serum ferritin falls consistently below 500 mcg/L, consider temporarily interrupting therapy with Exjade.
Based on Serum Creatinine
For adults, reduce the daily dose of Exjade by 10 mg/kg if a rise in serum creatinine to >33% above the average of the pretreatment measurements is seen at 2 consecutive visits, and cannot be attributed to other causes. For pediatric patients, reduce the dose by 10 mg/kg if serum creatinine levels rise above the age-appropriate upper limit of normal at 2 consecutive visits.
Concomitant UGT inducers or Cholestyramine
Concomitant use of UGT inducers or cholestyramine decreases deferasirox systemic exposure (AUC). Avoid the concomitant use of cholestyramine or potent UGT inducers (e.g., rifampicin, phenytoin, phenobarbital, ritonavir) with Exjade. If you must co-administer these agents together, consider increasing the initial dose of Exjade to 30 mg/kg, and monitor serum ferritin levels and clinical responses for further dose modification [see Drug Interactions (7.4, 7.5)].
Hepatic Impairment
Avoid the use of Exjade in patients with severe (Child-Pugh C) hepatic impairment. Reduce the starting dose by 50% in patients with moderate (Child-Pugh B) hepatic impairment. Closely monitor patients with mild (Child-Pugh A) or moderate (Child-Pugh B) hepatic impairment for efficacy and adverse reactions that may require dose titration [see Warnings and Precautions (5.2), and Use in Specific Populations (8.7).
Dosage Forms and Strengths
125 mg tablets
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “125” on one side and “NVR” on the other.
250 mg tablets
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “250” on one side and “NVR” on the other.
500 mg tablets
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “500” on one side and “NVR” on the other.
Contraindications
Exjade is contraindicated in patients with:
- creatinine clearance <40 mL/min or serum creatinine >2 times the age-appropriate upper limit of normal;
- poor performance status and high-risk myelodysplastic syndromes or advanced malignancies [see Warnings and Precautions (5.7)];
- platelet counts <50 x 109/L;
- known hypersensitivity to deferasirox or any component of Exjade.
Warnings and Precautions
Renal
Acute renal failure, fatal in some patients and requiring dialysis in others, has been reported following the postmarketing use of Exjade (deferasirox). Most fatalities occurred in patients with multiple comorbidities and who were in advanced stages of their hematological disorders. Monitor serum creatinine and/or creatinine clearance in patients who: are at increased risk of complications, have preexisting renal conditions, are elderly, have comorbid conditions, or are receiving medicinal products that depress renal function. Closely monitor the renal function of patients with creatinine clearances between 40 and less than 60 mL/min, particularly in situations where patients have additional risk factors that may further impair renal function such as concomitant medications, dehydration, or severe infections.
Assess serum creatinine and/or creatinine clearance in duplicate before initiating therapy to establish a reliable pretreatment baseline, due to variations in measurements. Monitor serum creatinine and/or creatinine clearance monthly thereafter. In patients with additional renal risk factors (see above), monitor serum creatinine and/or creatinine clearance weekly during the first month after initiation or modification of therapy and monthly thereafter.
Consider dose reduction, interruption, or discontinuation for increases in serum creatinine. If there is a progressive increase in serum creatinine beyond the age-appropriate upper limit of normal, interrupt Exjade use. Once the creatinine has returned to within the normal range, therapy with Exjade may be reinitiated at a lower dose followed by gradual dose escalation, if the clinical benefit is expected to outweigh potential risks [see Dose Modifications (2.2)].
In the clinical studies, for increases of serum creatinine on 2 consecutive measures (>33% in patients >15 years of age or >33% and greater than the age-appropriate upper limit of normal in patients <15 years of age), the daily dose of Exjade was reduced by 10 mg/kg. Patients with baseline serum creatinine above the upper limit of normal were excluded from clinical studies.
In the clinical studies, Exjade-treated patients experienced dose-dependent increases in serum creatinine. These increases occurred at a greater frequency compared to deferoxamine-treated patients (38% vs. 14%, respectively, in Study 1 and 36% vs 22%, respectively, in Study 3). Most of the creatinine elevations remained within the normal range [see Adverse Reactions (6.1)]. There have also been reports of renal tubulopathy in patients treated with Exjade. The majority of these patients were children and adolescents with ß-thalassemia and serum ferritin levels <1500 mcg/L.
Hepatic Dysfunction and Failure
Avoid the use of Exjade in patients with severe (Child-Pugh C) hepatic impairment. For patients with moderate (Child-Pugh B) hepatic impairment, a 50% reduction in the starting dose is recommended [see Dosage and Administration (2.2), and Use in Specific Populations (8.7)]. Closely monitor patients with mild (Child-Pugh A) or moderate (Child-Pugh B) hepatic impairment for efficacy and adverse reactions that may require dose titration.
In Study 1, 4 patients discontinued Exjade because of hepatic abnormalities (drug-induced hepatitis in 2 patients and increased serum transaminases in 2 additional patients). There have been postmarketing reports of hepatic failure, some with a fatal outcome, in patients treated with Exjade. Most of these events occurred in patients greater than 55 years of age. Most reports of hepatic failure involved patients with significant comorbidities, including liver cirrhosis and multiorgan failure. Serum transaminases and bilirubin should be monitored before the initiation of treatment, every 2 weeks during the first month and monthly thereafter. Consider dose modifications or interruption of treatment for severe or persistent elevations.
Gastrointestinal
Fatal GI hemorrhages, especially in elderly patients who had advanced hematologic malignancies and/or low platelet counts, have been reported. Non-fatal upper GI irritation, ulceration and hemorrhage have been reported in patients, including children and adolescents, receiving Exjade [see Adverse Reactions (6.1)]. Physicians and patients should remain alert for signs and symptoms of GI ulceration and hemorrhage during Exjade therapy and promptly initiate additional evaluation and treatment if a serious GI adverse event is suspected. Use caution when administering Exjade in combination with drugs that have ulcerogenic or hemorrhagic potential, such as non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroids, oral bisphosphonates, or anticoagulants.
Cytopenias
There have been postmarketing reports (both spontaneous and from clinical trials) of cytopenias, including agranulocytosis, neutropenia and thrombocytopenia, in patients treated with Exjade. Some of these patients died. The relationship of these episodes to treatment with Exjade is uncertain. Most of these patients had preexisting hematologic disorders that are frequently associated with bone marrow failure [see Adverse Reactions (6.2)]. Monitor blood counts regularly. Consider interrupting treatment with Exjade in patients who develop unexplained cytopenia. Reintroduction of therapy with Exjade may be considered, once the cause of the cytopenia has been elucidated.
Hypersensitivity
Serious hypersensitivity reactions (such as anaphylaxis and angioedema) have been reported in patients receiving Exjade, with the onset of the reaction occurring in the majority of cases within the first month of treatment [see Adverse Reactions (6.2)]. If reactions are severe, discontinue Exjade and institute appropriate medical intervention.
Rash
Rashes may occur during Exjade (deferasirox) treatment. For rashes of mild to moderate severity, Exjade may be continued without dose adjustment, since the rash often resolves spontaneously. In severe cases, Exjade may be interrupted. Reintroduction at a lower dose with escalation may be considered in combination with a short period of oral steroid administration. Erythema multiforme has been reported during Exjade treatment.
Co-morbidities
Clinical trials to demonstrate increased survival or to confirm clinical benefit have not been completed. Exjade has been shown to decrease serum ferritin and liver iron concentration in clinical trials. Consider the importance of these factors as well as individual patient factors and the prognosis associated with any underlying conditions before initiation of Exjade therapy [see Contraindications (4)].
In postmarketing experience, there have been reports of serious adverse reactions, some with a fatal outcome, in patients taking Exjade therapy, predominantly when the drug was administered to patients with advanced age, complications from underlying conditions or very advanced disease. Most of these deaths occurred within six months of Exjade initiation and generally involved worsening of the underlying condition. The reports do not rule out the possibility that Exjade may have contributed to the deaths.
Special Senses
Auditory disturbances (high frequency hearing loss, decreased hearing), and ocular disturbances (lens opacities, cataracts, elevations in intraocular pressure, and retinal disorders) have been reported at a frequency of <1% with Exjade therapy in the clinical studies. Auditory and ophthalmic testing (including slit lamp examinations and dilated fundoscopy) are recommended before starting Exjade treatment and thereafter at regular intervals (every 12 months). If disturbances are noted, consider dose reduction or interruption.
Laboratory Tests
Measure serum ferritin monthly to assess response to therapy and to evaluate for the possibility of overchelation of iron. If the serum ferritin falls consistently below 500 mcg/L, consider temporarily interrupting therapy with Exjade [see Dosage and Administration (2.2)].
In the clinical studies, the correlation coefficient between the serum ferritin and LIC was 0.63. Therefore, changes in serum ferritin levels may not always reliably reflect changes in LIC.
Perform laboratory monitoring of renal and hepatic function [see Warnings and Precautions (5.1, 5.3)].
Adverse Reactions
Clinical Trials Experience
The following adverse reactions are also discussed in other sections of the labeling:
Renal Failure [see Warnings and Precautions (5.1)]. Hepatic Failure [see Warnings and Precautions (5.2)]. Fatal and non-fatal Gastrointestinal Bleedings [see Warnings and Precautions (5.3)]. Cytopenias [see Warnings and Precautions (5.4)].
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
A total of 700 adult and pediatric patients were treated with Exjade (deferasirox) for 48 weeks in premarketing studies. These included 469 patients with ß-thalassemia, 99 with rare anemias, and 132 with sickle cell disease. Of these patients, 45% were male, 70% were Caucasian and 292 patients were < 16 years of age. In the sickle cell disease population, 89% of patients were Black. Median treatment duration among the sickle cell patients was 51 weeks. Of the 700 patients treated, 469 (403 ß-thalassemia and 66 rare anemias) were entered into extensions of the original clinical protocols. In ongoing extension studies, median durations of treatment were 88-205 weeks.
Table 1 displays adverse reactions occurring in >5% of Exjade-treated β-thalassemia patients (Study 1) and sickle cell disease patients (Study 3) with a suspected relationship to study drug. Abdominal pain, nausea, vomiting, diarrhea, skin rashes, and increases in serum creatinine were the most frequent adverse reactions reported with a suspected relationship to Exjade. Gastrointestinal symptoms, increases in serum creatinine, and skin rash were dose related.
| Study 1 (ß-Thalassemia) | Study 3 (Sickle Cell Disease) | ||||
| Preferred Term | Exjade N=296 n (%) |
Deferoxamine N=290 n (%) |
Exjade N=132 n (%) |
Deferoxamine N=63 n (%) | |
| Abdominal Pain** | 63 (21.3) | 41 (14.1) | 37 (28.0) | 9 (14.3) | |
| Diarrhea | 35 (11.8) | 21 (7.2) | 26 (19.7) | 3 (4.8) | |
| Creatinine Increased*** | 33 (11.1) | 0 (0) | 9 (6.8) | 0 | |
| Nausea | 31 (10.5) | 14 (4.8) | 30 (22.7) | 7 (11.1) | |
| Vomiting | 30 (10.1) | 28 (9.7) | 28 (21.2) | 10 (15.9) | |
| Rash | 25 (8.4) | 9 (3.1) | 14 (10.6) | 3 (4.8) | |
| *Adverse reaction frequencies are based on adverse events reported regardless of relationship to study drug. ** Includes ‘abdominal pain’, ‘abdominal pain lower’, and ‘abdominal pain upper’ which were reported as adverse events. *** Includes ‘blood creatinine increased’ and ‘blood creatinine abnormal’ which were reported as adverse events. Also see Table 2. | |||||
In Study 1, a total of 113 (38%) patients treated with Exjade had increases in serum creatinine >33% above baseline on 2 separate occasions (Table 2) and 25 (8%) patients required dose reductions. Increases in serum creatinine appeared to be dose related [see Warnings and Precautions (5.1)]. In this study, 17 (6%) patients treated with Exjade developed elevations in SGPT/ALT levels >5 times the upper limit of normal at 2 consecutive visits. Of these, 2 patients had liver biopsy proven drug-induced hepatitis and both discontinued Exjade therapy [see Warnings and Precautions (5.2)]. An additional 2 patients, who did not have elevations in SGPT/ALT >5 times the upper limit of normal, discontinued Exjade because of increased SGPT/ALT. Increases in transaminases did not appear to be dose related. Adverse reactions that led to discontinuations included abnormal liver function tests (2 patients) and drug-induced hepatitis (2 patients), skin rash, glycosuria/proteinuria, Henoch Schönlein purpura, hyperactivity/insomnia, drug fever, and cataract (1 patient each).
In Study 3, a total of 48 (36%) patients treated with Exjade had increases in serum creatinine >33% above baseline on 2 separate occasions (Table 2) [see Warnings and Precautions (5.1)]. Of the patients who experienced creatinine increases in Study 3, 8 Exjade-treated patients required dose reductions. In this study, 5 patients in the Exjade group developed elevations in SGPT/ALT levels >5 times the upper limit of normal at 2 consecutive visits and 1 patient subsequently had Exjade permanently discontinued. Four additional patients discontinued Exjade due to adverse reactions with a suspected relationship to study drug, including diarrhea, pancreatitis associated with gallstones, atypical tuberculosis, and skin rash.
Study 1 (ß-Thalassemia) |
Study 3 (Sickle Cell Disease) | ||||||
Laboratory Parameter |
Exjade N=296 n (%) |
Deferoxamine N=290 n (%) |
Exjade N=132 n (%) |
Deferoxamine N=63 n (%) | |||
| Serum Creatinine | |||||||
| Creatinine increase >33% and <ULN at 2 consecutive postbaseline visits | 113 (38.2) | 41 ( 14.1) | 48 (36.4) | 14 (22.2) | |||
| Creatinine increase >33% and >ULN at 2 consecutive postbaseline visits | 7 (2.4) | 1 (0.3) | 3 (2.3) | 2 (3.2) | |||
| SGPT/ALT | |||||||
| SGPT/ALT >5 x ULN at 2 postbaseline visits | 25 (8.4) | 7 (2.4) | 2 (1.5) | 0 | |||
| SGPT/ALT >5 x ULN at 2 consecutive postbaseline visits | 17 (5.7) | 5 (1.7) | 5 (3.8) | 0 | |||
Proteinuria
In clinical studies, urine protein was measured monthly. Intermittent proteinuria (urine protein/creatinine ratio >0.6 mg/mg) occurred in 18.6% of Exjade-treated patients compared to 7.2% of deferoxamine-treated patients in Study 1. Although no patients were discontinued from Exjade in clinical studies up to 1 year due to proteinuria, monthly monitoring is recommended. The mechanism and clinical significance of the proteinuria are uncertain.
Other Adverse Reactions
In the population of more than 5,000 patients who have been treated with Exjade during clinical trials, adverse reactions occurring in 0.1% to 1% of patients included gastritis, edema, sleep disorder, pigmentation disorder, dizziness, anxiety, maculopathy, cholelithiasis, pyrexia, fatigue, pharyngolaryngeal pain, early cataract, hearing loss, gastrointestinal hemorrhage, gastric ulcer (including multiple ulcers), duodenal ulcer, and renal tubulopathy (Fanconi’s syndrome). Adverse reactions occurring in 0.01% to 0.1% of patients included optic neuritis, esophagitis, and erythema multiforme. Adverse reactions which most frequently led to dose interruption or dose adjustment during clinical trials were rash, gastrointestinal disorders, infections, increased serum creatinine, and increased serum transaminases.
Postmarketing Experience
The following adverse reactions have been spontaneously reported during postapproval use of Exjade. Because these reactions are reported voluntarily from a population of uncertain size, in which patients may have received concomitant medication, it is not always possible to reliably estimate frequency or establish a causal relationship to drug exposure.
Skin and subcutaneous tissue disorders: leukocytoclastic vasculitis, urticaria, alopecia
Immune system disorders: hypersensitivity reactions (including anaphylaxis and angioedema).
Drug Interactions
The concomitant administration of Exjade and aluminum-containing antacid preparations has not been formally studied. Although deferasirox has a lower affinity for aluminum than for iron, do not administer Exjade with aluminum-containing antacid preparations.
Effect of Deferasirox on Drug Metabolizing Enzymes
Deferasirox inhibits human CYP3A4, CYP2C8, CYP1A2, CYP2A6, CYP2D6, and CYP2C19 in vitro. The clinical significance of deferasirox inhibition of CYP1A2, CYP2A6, CYP2D6, and CYP2C19 is unknown.
Interaction with Midazolam and Other Agents Metabolized by CYP3A4
In healthy volunteers, the concomitant administration of Exjade and midazolam (a CYP3A4 probe substrate) resulted in a decrease of midazolam peak concentration by 23 % and exposure by 17%. In the clinical setting, this effect may be more pronounced. Therefore, due to a possible decrease in CYP3A4 substrate concentration and potential loss of effectiveness, use caution when deferasirox is administered with drugs metabolized by CYP3A4 (e.g., cyclosporine, simvastatin, hormonal contraceptive agents).
Interaction with Repaglinide and Other Agents Metabolized by CYP2C8
In a healthy volunteer study, the concomitant administration of Exjade (30 mg/kg/day for 4 days) and the CYP2C8 probe substrate repaglinide (single dose of 0.5 mg) resulted in an increase in repaglinide systemic exposure (AUC) to 2.3-fold of control and an increase in Cmax of 62%. If Exjade and repaglinide are used concomitantly, consider decreasing the dose of repaglinide and perform careful monitoring of blood glucose levels. Exercise caution when Exjade and other CYP2C8 substrates like paclitaxel are co-administered.
Interaction with Theophylline and Other Agents Metabolized by CYP1A2
In a healthy volunteer study, the concomitant administration of Exjade (repeated dose of 30 mg/kg/day) and the CYP1A2 substrate theophylline (single dose of 120 mg) resulted in an approximate doubling of the theophylline AUC and elimination half-life. The single dose Cmax was not affected, but an increase in theophylline Cmax is expected to occur with chronic dosing. This increase in plasma concentrations could lead to clinically significant theophylline induced CNS or other adverse reactions. Avoid the concomitant use of theophylline or other CYP1A2 substrates with a narrow therapeutic index with Exjade. If you must co-administer theophylline with Exjade, monitor theophylline concentrations and consider theophylline dose modification.
Use caution when Exjade is administered with other drugs metabolized by CYP1A2 such as cyclobenzaprine, imipramine, haloperidol, fluvoxamine, mexiletine, olanzapine, tizanidine, zileuton, and zolmitriptan.
Interaction with Agents Inducing UDP-glucuronosyltransferase (UGT) Metabolism
In a healthy volunteer study, the concomitant administration of Exjade (single dose of 30 mg/kg) and the potent UDP-glucuronosyltransferase (UGT) inducer rifampicin (600 mg/day for 9 days) resulted in a decrease of deferasirox systemic exposure (AUC) by 44%. Therefore, the concomitant use of Exjade with potent UGT inducers (e.g., rifampicin, phenytoin, phenobarbital, ritonavir) may result in a decrease in Exjade efficacy.
Avoid the concomitant use of potent UGT inducers with Exjade. If you must co-administer these agents together, consider increasing the initial dose of Exjade to 30 mg/kg and monitor serum ferritin levels and clinical responses for further dose modification [see Dosage and Administration (2.2)].
Interaction with Cholestyramine
The concomitant use of Exjade with cholestyramine may result in a decrease in Exjade efficacy. In healthy volunteers, the administration of cholesytramine after a single dose of deferasirox resulted in a 45% decrease in deferasirox exposure (AUC). Avoid the concomitant use of cholestyramine with Exjade. If you must co-administer these agents together, consider increasing the initial dose of Exjade to 30 mg/kg and monitor serum ferritin levels and clinical responses for further dose modification [see Dosage and Administration (2.2)].
USE IN SPECIFIC POPULATIONS
Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies with Exjade in pregnant women. Administration of deferasirox to animals during pregnancy and lactation resulted in decreased offspring viability and an increase in renal anomalies in male offspring at exposures that were less than the recommended human exposure. Exjade should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
In embryofetal developmental studies, pregnant rats and rabbits received oral deferasirox during the period of organogenesis at doses up to (100 mg/kg/day in rats and 50 mg/kg/day in rabbits) 0.8 times the MRHD (Maximum Recommended Human Dose) on a mg/m2 basis. These doses resulted in maternal toxicity but no fetal harm was observed.
In a prenatal and postnatal developmental study, pregnant rats received oral deferasirox daily from organogenesis through lactation day 20 at doses (10, 30, and 90 mg/kg/day) 0.08, 0.2, and 0.7 times the MRHD on a mg/m2 basis. Maternal toxicity, loss of litters, and decreased offspring viability occurred at 0.7 times the MRHD on a mg/m2 basis, and increases in renal anomalies in male offspring occurred at 0.2 times the MRHD on a mg/m2 basis.
Nursing Mothers
It is not known whether Exjade is excreted in human milk. Deferasirox and its metabolites were excreted in rat milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from deferasirox and its metabolites, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Of the 700 patients who received Exjade during clinical studies, 292 were pediatric patients 2 - <16 years of age with various congenital and acquired anemias, including 52 patients age 2 - <6 years, 121 patients age 6 - <12 years and 119 patients age 12 - <16 years. Seventy percent of these patients had β-thalassemia. Children between the ages of 2 - <6 years have a systemic exposure to Exjade approximately 50% of that of adults [see Clinical Pharmacology (12.3)]. However, the safety and efficacy of Exjade in pediatric patients was similar to that of adult patients, and younger pediatric patients responded similarly to older pediatric patients. The recommended starting dose and dosing modification are the same for children and adults [see Clinical Studies (14), Indications and Usage (1), and Dosage and Administration (2.1)].
Growth and development were within normal limits in children followed for up to 5 years in clinical trials.
Geriatric Use
Four hundred and thirty-one (431) patients ≥65 years of age have been studied in clinical trials of Exjade. The majority of these patients had myelodysplastic syndrome (MDS) (n=393). In these trials, elderly patients experienced a higher frequency of adverse reactions than younger patients. Closely monitor elderly patients for early signs or symptoms of adverse reactions that may require a dose adjustment. Elderly patients are at increased risk for Exjade toxicity due to the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Renal Impairment
Exjade has not been studied in patients with renal impairment [see Warnings and Precautions (5.1)].
Hepatic Impairment
In a single dose (20 mg/kg) study in patients with varying degrees of hepatic impairment, deferasirox exposure was increased compared to patients with normal hepatic function. The average total (free and bound) AUC of deferasirox increased 16% in 6 subjects with mild (Child-Pugh A) hepatic impairment, and 76% in 6 subjects with moderate (Child-Pugh B) hepatic impairment compared to 6 subjects with normal hepatic function. The impact of severe (Child-Pugh C) hepatic impairment was assessed in only one subject.
Avoid the use of Exjade in patients with severe (Child-Pugh C) hepatic impairment. For patients with moderate (Child-Pugh B) hepatic impairment, the starting dose should be reduced by 50%. Closely monitor patients with mild (Child-Pugh A) or moderate (Child-Pugh B) hepatic impairment for efficacy and adverse reactions that may require dose titration [See Dosage and Administration (2.2), and Warnings and Precautions (5.2].
Overdosage
Cases of overdose (2-3 times the prescribed dose for several weeks) have been reported. In one case, this resulted in hepatitis which resolved without long-term consequences after a dose interruption. Single doses up to 80 mg/kg/day in iron overloaded β-thalassemic patients have been tolerated with nausea and diarrhea noted. In healthy volunteers, single doses of up to 40 mg/kg/day were tolerated. There is no specific antidote for Exjade. In case of overdose, induce vomiting and employ gastric lavage.
Exjade Description
Exjade (deferasirox) is an iron chelating agent. Exjade tablets for oral suspension contain 125 mg, 250 mg, or 500 mg deferasirox. Deferasirox is designated chemically as 4-[3,5-Bis (2-hydroxyphenyl)-1H-1,2,4-triazol-1-yl]-benzoic acid and its structural formula is
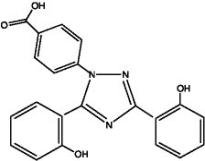
Deferasirox is a white to slightly yellow powder. Its molecular formula is C21H15N3O4 and its molecular weight is 373.4.
Inactive Ingredients: Lactose monohydrate (NF), crospovidone (NF), povidone (K30) (NF), sodium lauryl sulphate (NF), microcrystalline cellulose (NF), silicon dioxide (NF), and magnesium stearate (NF).
Exjade - Clinical Pharmacology
Mechanism of Action
Exjade (deferasirox) is an orally active chelator that is selective for iron (as Fe3+). It is a tridentate ligand that binds iron with high affinity in a 2:1 ratio. Although deferasirox has very low affinity for zinc and copper there are variable decreases in the serum concentration of these trace metals after the administration of deferasirox. The clinical significance of these decreases is uncertain.
Pharmacodynamics
Pharmacodynamic effects tested in an iron balance metabolic study showed that deferasirox (10, 20 and 40 mg/kg per day) was able to induce a mean net iron excretion (0.119, 0.329 and 0.445 mg Fe/kg body weight per day, respectively) within the clinically relevant range (0.1-0.5 mg/kg per day). Iron excretion was predominantly fecal.
Pharmacokinetics
Absorption
Exjade is absorbed following oral administration with median times to maximum plasma concentration (tmax) of about 1.5-4 hours. The Cmax and AUC of deferasirox increase approximately linearly with dose after both single administration and under steady-state conditions. Exposure to deferasirox increased by an accumulation factor of 1.3-2.3 after multiple doses. The absolute bioavailability (AUC) of deferasirox tablets for oral suspension is 70% compared to an intravenous dose. The bioavailability (AUC) of deferasirox was variably increased when taken with a meal.
Distribution
Deferasirox is highly (~99%) protein bound almost exclusively to serum albumin. The percentage of deferasirox confined to the blood cells was 5% in humans. The volume of distribution at steady state (Vss) of deferasirox is 14.37 ± 2.69 L in adults.
Metabolism
Glucuronidation is the main metabolic pathway for deferasirox, with subsequent biliary excretion. Deconjugation of glucuronidates in the intestine and subsequent reabsorption (enterohepatic recycling) is likely to occur. Deferasirox is mainly glucuronidated by UGT1A1 and to a lesser extent UGT1A3. CYP450-catalyzed (oxidative) metabolism of deferasirox appears to be minor in humans (about 8%). Deconjugation of glucuronide metabolites in the intestine and subsequent reabsorption (enterohepatic recycling) was confirmed in a healthy volunteer study in which the administration of cholestyramine 12 g twice daily (strongly binds to deferasirox and its conjugates) 4 and 10 hours after a single dose of deferasirox resulted in a 45% decrease in deferasirox exposure (AUC) by interfering with the enterohepatic recycling of deferasirox.
Excretion
Deferasirox and metabolites are primarily (84% of the dose) excreted in the feces. Renal excretion of deferasirox and metabolites is minimal (8% of the administered dose). The mean elimination half-life (t1/2) ranged from 8-16 hours following oral administration.
Pharmacokinetics in Special Populations
Pediatric: Following oral administration of single or multiple doses, systemic exposure of adolescents and children to deferasirox was less than in adult patients. In children <6 years of age, systemic exposure was about 50% lower than in adults.
Geriatric: The pharmacokinetics of deferasirox have not been studied in geriatric patients (65 years of age or older).
Gender: Females have a moderately lower apparent clearance (by 17.5%) for deferasirox compared to males.
Renal Insufficiency: Deferasirox is minimally (8%) excreted via the kidney.
Hepatic Impairment: Deferasirox is principally excreted by glucuronidation and is minimally (8%) metabolized by oxidative cytochrome P450 enzymes. Exjade treatment has been initiated in patients with baseline liver transaminase levels up to 5 times the upper limit of the normal range. The pharmacokinetics of deferasirox were not influenced by such transaminase levels.
The average AUC of deferasirox in 6 subjects with mild hepatic impairment (Child-Pugh A) increased 16% over that found in 6 subjects with normal hepatic function, while the average AUC of deferasirox in 6 subjects with moderate hepatic impairment (Child-Pugh B) increased 76% over that found in 6 subjects with normal hepatic function. The average Cmax of deferasirox in subjects with mild or moderate hepatic impairment increased 22% over that found in subjects with normal hepatic function. The impact of severe hepatic impairment (Child-Pugh C) was assessed in only one subject [see Dosage and Administration (2.2), Warnings and Precautions (5.2), and Use in Specific Populations (8.7)].
QT Prolongation
The effect of 20 and 40 mg/kg per day of deferasirox on the QT interval was evaluated in a single-dose, double-blind, randomized, placebo- and active-controlled (moxifloxacin 400 mg), parallel group study in 182 healthy male and female volunteers age 18-65 years. No evidence of prolongation of the QTc interval was observed in this study.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
A 104-week oral carcinogenicity study in Wistar rats showed no evidence of carcinogenicity from deferasirox at doses up to 60 mg/kg per day (0.48 times the MRHD (Maximum Recommended Human Dose) on a mg/m2 basis). A 26-week oral carcinogenicity study in p53 (+/-) transgenic mice has shown no evidence of carcinogenicity from deferasirox at doses up to 200 mg/kg per day (0.81 times the MRHD on a mg/m2 basis) in males and 300 mg/kg per day (1.21 times the MRHD on a mg/m2 basis) in females.
Deferasirox was negative in the Ames test and chromosome aberration test with human peripheral blood lymphocytes. It was positive in 1 of 3 in-vivo oral rat micronucleus tests.
Deferasirox at oral doses up to 75 mg/kg per day (0.6 times the MRHD on a mg/m2 basis) was found to have no adverse effect on fertility and reproductive performance of male and female rats.
Clinical Studies
The primary efficacy study, Study 1, was a multicenter, open-label, randomized, active comparator control study to compare Exjade (deferasirox) and deferoxamine in patients with β-thalassemia and transfusional hemosiderosis. Patients ≥2 years of age were randomized in a 1:1 ratio to receive either oral Exjade at starting doses of 5, 10, 20 or 30 mg/kg once daily or subcutaneous Desferal (deferoxamine) at starting doses of 20 to 60 mg/kg for at least 5 days per week based on LIC (liver iron concentration) at baseline (2-3, >3-7, >7-14 and >14 mg Fe/g dry weight). Patients randomized to deferoxamine who had LIC values <7 mg Fe/g dry weight were permitted to continue on their prior deferoxamine dose, even though the dose may have been higher than specified in the protocol.
Patients were to have a liver biopsy at baseline and end of study (after 12 months) for LIC. The primary efficacy endpoint was defined as a reduction in LIC of ≥3 mg Fe/g dry weight for baseline values ≥10 mg Fe/g dry weight, reduction of baseline values between 7 and <10 to <7 mg Fe/g dry weight, or maintenance or reduction for baseline values <7 mg Fe/g dry weight.
A total of 586 patients were randomized and treated, 296 with Exjade and 290 with deferoxamine. The mean age was 17.1 years (range, 2-53 years); 52% were females and 88% were Caucasian. The primary efficacy population consisted of 553 patients (Exjade n=276; deferoxamine n=277) who had LIC evaluated at baseline and 12 months or discontinued due to an adverse event. The percentage of patients achieving the primary endpoint was 52.9% for Exjade and 66.4% for deferoxamine. The relative efficacy of Exjade to deferoxamine cannot be determined from this study.
In patients who had an LIC at baseline and at end of study, the mean change in LIC was -2.4 mg Fe/g dry weight in patients treated with Exjade and -2.9 mg Fe/g dry weight in patients treated with deferoxamine.
Reduction of LIC and serum ferritin was observed with Exjade doses of 20 to 30 mg/kg per day. Exjade doses below 20 mg/kg per day failed to provide consistent lowering of LIC and serum ferritin levels (Figure 1). Therefore, a starting dose of 20 mg/kg per day is recommended [see Dosage and Administration (2.1)].

Figure 1. Changes in Liver Iron Concentration and Serum Ferritin Following Exjade (5-30 mg/kg per day) in Study 1
Study 2 was an open-label, noncomparative trial of efficacy and safety of Exjade given for 1 year to patients with chronic anemias and transfusional hemosiderosis. Similar to Study 1, patients received 5, 10, 20, or 30 mg/kg per day of Exjade based on baseline LIC.
A total of 184 patients were treated in this study: 85 patients with β-thalassemia and 99 patients with other congenital or acquired anemias (myelodysplastic syndromes, n=47; Diamond-Blackfan syndrome, n=30; other, n=22). 19% of patients were <16 years of age and 16% were ≥65 years of age. There was a reduction in the absolute LIC from baseline to end of study (-4.2 mg Fe/g dry weight).
Study 3 was a multicenter, open-label, randomized trial of the safety and efficacy of Exjade relative to deferoxamine given for 1 year in patients with sickle cell disease and transfusional hemosiderosis. Patients were randomized to Exjade at doses of 5, 10, 20, or 30 mg/kg per day or subcutaneous deferoxamine at doses of 20-60 mg/kg per day for 5 days per week according to baseline LIC.
A total of 195 patients were treated in this study: 132 with Exjade and 63 with deferoxamine. 44% of patients were <16 years of age and 91% were Black. At end of study, the mean change in LIC (as measured by magnetic susceptometry by a superconducting quantum interference device) in the per protocol-1 (PP-1) population, which consisted of patients who had at least one postbaseline LIC assessment, was -1.3 mg Fe/g dry weight for patients receiving Exjade (n=113) and -0.7 mg Fe/g dry weight for patients receiving deferoxamine (n=54).
How Supplied/Storage and Handling
Exjade is provided as 125 mg, 250 mg, and 500 mg tablets for oral suspension.
125 mg
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “125” on one side and “NVR” on the other.
Bottles of 30 tablets………………………………………………………………..(NDC 0078 - 0468 - 15)
250 mg
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “250” on one side and “NVR” on the other.
Bottles of 30 tablets………………………………………………………………..(NDC 0078 - 0469 - 15)
500 mg
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “500” on one side and “NVR” on the other.
Bottles of 30 tablets………………………………………………………………..(NDC 0078 - 0470 - 15)
Store Exjade tablets at 25°C (77°F); excursions are permitted to 15–30°C (59–86°F) [see USP Controlled Room Temperature]. Protect from moisture.
Patient Counseling Information
Advise patients to take Exjade once daily on an empty stomach at least 30 minutes prior to food, preferably at the same time every day. Instruct patients to completely disperse the tablets in water, orange juice, or apple juice, and drink the resulting suspension immediately. After the suspension has been swallowed, resuspend any residue in a small volume of the liquid and swallow.
Advise patients not to chew tablets or swallow them whole.
Advise patients who experience diarrhea or vomiting to maintain adequate hydration.
Caution patients not to take aluminum-containing antacids and Exjade simultaneously.
Because auditory and ocular disturbances have been reported with Exjade, conduct auditory testing and ophthalmic testing before starting Exjade treatment and thereafter at regular intervals [see Warnings and Precautions (5.8)].
Caution patients experiencing dizziness to avoid driving or operating machinery [see Adverse Reactions (6.1)].
Caution patients about the potential for the development of GI ulcers or bleeding when taking Exjade in combination with drugs that have ulcerogenic or hemorrhagic potential, such as NSAIDs, corticosteroids, oral bisphosphonates, or anticoagulants.
Caution patients about potential loss of effectiveness of drugs metabolized by CYP3A4 (e.g., cyclosporine, simvastatin, hormonal contraceptive agents) when Exjade is administered with these drugs.
Caution patients about potential loss of effectiveness of Exjade when administered with drugs that are potent UGT inducers (e.g., rifampicin, phenytoin, phenobarbital, ritonavir). Based on serum ferritin levels and clinical response, consider increases in the dose of Exjade when concomitantly used with potent UGT inducers.
Perform careful monitoring of glucose levels when repaglinide is used concomitantly with Exjade. An interaction between Exjade and other CYP2C8 substrates like paclitaxel cannot be excluded.
Advise patients that blood tests will be performed because Exjade may affect your kidneys, liver, or blood. The blood tests will be performed every month or more frequently if you are at increased risk of complications (e.g., pre-existing kidney condition, are elderly, have multiple medical conditions, or are taking medicine that affects your organs). There have been reports of severe kidney and liver problems, blood disorders, stomach bleeds and death in patients taking Exjade.
Skin rashes may occur during Exjade treatment and if severe treatment should be interrupted. Serious allergic reactions (which include swelling of the throat) have been reported in patients taking Exjade, usually within the first month of treatment. If reactions are severe, advise patients to stop taking Exjade and contact their doctor immediately.
Certain patients should not receive Exjade. These include patients with severe (Child-Pugh C) hepatic impairment, creatinine clearance <40 mL/min or serum creatinine >2 times the age-appropriate upper limit of normal, patients with poor performance status and high-risk myelodysplastic syndromes or advanced malignancies, patients with platelet counts <50 x 109/L, and those with hypersensitivity to deferasirox or any component of Exjade.
Manufactured by:
Novartis Pharma Stein AG
Stein, Switzerland
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
© Novartis
T2011-106
PRINCIPAL DISPLAY PANEL
Package Label – 125 mg Tablets for Oral Suspension
Rx Only NDA 0078-0468-15
Exjade® (deferasirox)
Tablets for Oral Suspension
125 mg per tablet
30 Tablets
DO NOT CHEW OR SWALLOW WHOLE
*Tablets MUST be dispersed in water,
orange or apple juice prior to ingestion.