|
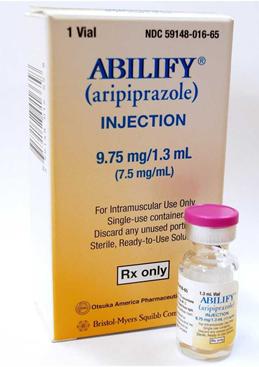
英文药名: Abilify(Aripiprazole Tablets) 中文药名: 阿立哌唑片 生产厂家: 大冢制药/百时美施贵宝
Extrapyramidal symptoms (EPS) Schizophrenia: in a long term 52-week controlled trial, aripiprazole-treated patients had an overall-lower incidence (25.8 %) of EPS including parkinsonism, akathisia, dystonia and dyskinesia compared with those treated with haloperidol (57.3 %). In a long term 26-week placebo-controlled trial, the incidence of EPS was 19 % for aripiprazole-treated patients and 13.1 % for placebo-treated patients. In another long-term 26-week controlled trial, the incidence of EPS was 14.8 % for aripiprazole-treated patients and 15.1 % for olanzapine-treated patients. Manic episodes in Bipolar I Disorder - in a 12-week controlled trial, the incidence of EPS was 23.5 % for aripiprazole-treated patients and 53.3 % for haloperidol-treated patients. In another 12-week trial, the incidence of EPS was 26.6 % for patients treated with aripiprazole and 17.6 % for those treated with lithium. In the long term 26-week maintenance phase of a placebo-controlled trial, the incidence of EPS was 18.2 % for aripiprazole-treated patients and 15.7 % for placebo-treated patients. Akathisia In placebo-controlled trials, the incidence of akathisia in bipolar patients was 12.1 % with aripiprazole and 3.2 % with placebo. In schizophrenia patients the incidence of akathisia was 6.2 % with aripiprazole and 3.0 % with placebo. Dystonia Class Effect - Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups. Comparisons between aripiprazole and placebo in the proportions of patients experiencing potentially clinically significant changes in routine laboratory and lipid parameters (see section 5.1) revealed no medically important differences. Elevations of CPK (Creatine Phosphokinase), generally transient and asymptomatic, were observed in 3.5 % of aripiprazole treated patients as compared to 2.0 % of patients who received placebo. Other findings Adverse reactions known to be associated with antipsychotic therapy and also reported during treatment with aripiprazole include neuroleptic malignant syndrome, tardive dyskinesia, seizure, cerebrovascular adverse reactions and increased mortality in elderly demented patients, hyperglycaemia and diabetes mellitus (see section 4.4). Paediatric population Schizophrenia in adolescents aged 15 years and older In a short-term placebo-controlled clinical trial involving 302 adolescents (13-17 years) with schizophrenia, the frequency and type of undesirable effects were similar to those in adults except for the following reactions that were reported more frequently in adolescents receiving aripiprazole than in adults receiving aripiprazole (and more frequently than placebo): somnolence/sedation and extrapyramidal disorder were reported very commonly (≥ 1/10), and dry mouth, increased appetite, and orthostatic hypotension were reported commonly (≥ 1/100, < 1/10). The safety profile in a 26-week open-label extension trial was similar to that observed in the short-term, placebo-controlled trial. In the pooled adolescent schizophrenia population (13-17 years) with exposure up to 2 years, incidence of low serum prolactin levels in females (<3 ng/ml) and males (<2 ng/ml) was 29.5 % and 48.3 %, respectively. In the adolescent (13-17 years) schizophrenia population with aripiprazole exposure of 5 to 30 mg up to 72 months, incidence of low serum prolactin levels in females (<3 ng/ml) and males (<2 ng/ml) was 25.6 % and 45.0 %, respectively. Manic episodes in Bipolar I Disorder in adolescents aged 13 years and older The frequency and type of undesirable effects in adolescents with Bipolar I Disorder were similar to those in adults except for the following reactions: very commonly (≥ 1/10) somnolence (23.0 %), extrapyramidal disorder (18.4 %), akathisia (16.0 %), and fatigue (11.8 %); and commonly (≥ 1/100, < 1/10) abdominal pain upper, heart rate increased, weight increased, increased appetite, muscle twitching, and dyskinesia. The following undesirable effects had a possible dose response relationship; extrapyramidal disorder (incidences were 10 mg, 9.1 %, 30 mg, 28.8 %, placebo, 1.7 %,); and akathisia (incidences were 10 mg, 12.1 %, 30 mg, 20.3 %, placebo, 1.7 %). Mean changes in body weight in adolescents with Bipolar I Disorder at 12 and 30 weeks for aripiprazole were 2.4 kg and 5.8 kg, and for placebo 0.2 kg and 2.3 kg, respectively. In the paediatric population somnolence and fatigue were observed more frequently in patients with bipolar disorder compared to patients with schizophrenia. In the paediatric bipolar population (10-17 years) with exposure up to 30 weeks, incidence of low serum prolactin levels in females (<3 ng/ml) and males (<2 ng/ml) was 28.0 % and 53.3 %, respectively. Post-Marketing The following adverse reactions have been reported during post-marketing surveillance. The frequency of these reactions is considered not known (cannot be estimated from the available data). Blood and lymphatic system disorders: leukopenia, neutropenia, thrombocytopenia Immune system disorders: allergic reaction (e.g. anaphylactic reaction, angioedema including swollen tongue, tongue oedema, face oedema, pruritus, or urticaria) Endocrine disorders: hyperglycaemia, diabetes mellitus, diabetic ketoacidosis, diabetic hyperosmolar coma Metabolism and nutrition disorders: weight gain, weight decreased, anorexia, hyponatremia Psychiatric disorders: agitation, nervousness, pathological gambling; suicide attempt, suicidal ideation, and completed suicide (see section 4.4) Nervous system disorders: speech disorder, Neuroleptic Malignant Syndrome (NMS), grand mal convulsion, serotonin syndrome Cardiac disorders: QT prolongation, ventricular arrhythmias, sudden unexplained death, cardiac arrest, torsades de pointes, bradycardia Vascular disorders: syncope, hypertension, venous thromboembolism (including pulmonary embolism and deep vein thrombosis) Respiratory, thoracic and mediastinal disorders: oropharyngeal spasm, laryngospasm, aspiration pneumonia Gastrointestinal disorders: pancreatitis, dysphagia, abdominal discomfort, stomach discomfort, diarrhoea Hepatobiliary disorders: hepatic failure, jaundice, hepatitis, increased Alanine Aminotransferase (ALT), increased Aspartate Aminotransferase (AST), increased Gamma Glutamyl Transferase (GGT), increased alkaline phosphatase Skin and subcutaneous tissue disorders: rash, photosensitivity reaction, alopecia, hyperhidrosis Musculoskeletal and connective tissue disorders: rhabdomyolysis, myalgia, stiffness Renal and urinary disorders: urinary incontinence, urinary retention Pregnancy, puerperium and perinatal conditions: drug withdrawal syndrome neonatal (see section 4.6) Reproductive system and breast disorders: priapism General disorders and administration site conditions: temperature regulation disorder (e.g. hypothermia, pyrexia), chest pain, peripheral oedema Investigations: increased Creatine Phosphokinase, blood glucose increased, blood glucose fluctuation, glycosylated haemoglobin increased Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via Yellow Card Scheme, Website: www.mhra.gov.uk/yellowcard. 4.9 Overdose Signs and symptoms In clinical trials and post-marketing experience, accidental or intentional acute overdose of aripiprazole alone was identified in adult patients with reported estimated doses up to 1,260 mg with no fatalities. The potentially medically important signs and symptoms observed included lethargy, increased blood pressure, somnolence, tachycardia, nausea, vomiting and diarrhoea. In addition, reports of accidental overdose with aripiprazole alone (up to 195 mg) in children have been received with no fatalities. The potentially medically serious signs and symptoms reported included somnolence, transient loss of consciousness and extrapyramidal symptoms. Management of overdose Management of overdose should concentrate on supportive therapy, maintaining an adequate airway, oxygenation and ventilation, and management of symptoms. The possibility of multiple medicinal product involvement should be considered. Therefore cardiovascular monitoring should be started immediately and should include continuous electrocardiographic monitoring to detect possible arrhythmias. Following any confirmed or suspected overdose with aripiprazole, close medical supervision and monitoring should continue until the patient recovers. Activated charcoal (50 g), administered one hour after aripiprazole, decreased aripiprazole Cmax by about 41 % and AUC by about 51 %, suggesting that charcoal may be effective in the treatment of overdose. Haemodialysis Although there is no information on the effect of haemodialysis in treating an overdose with aripiprazole, haemodialysis is unlikely to be useful in overdose management since aripiprazole is highly bound to plasma proteins. 5. Pharmacological properties 5.1 Pharmacodynamic properties Pharmacotherapeutic group: other antipsychotics, ATC code: N05AX12 Mechanism of action It has been proposed that aripiprazole's efficacy in schizophrenia and Bipolar I Disorder is mediated through a combination of partial agonism at dopamine D2 and serotonin 5HT1a receptors and antagonism of serotonin 5HT2a receptors. Aripiprazole exhibited antagonist properties in animal models of dopaminergic hyperactivity and agonist properties in animal models of dopaminergic hypoactivity. Aripiprazole exhibited high binding affinity in vitro for dopamine D2 and D3, serotonin 5HT1a and 5HT2a receptors and moderate affinity for dopamine D4, serotonin 5HT2c and 5HT7, alpha-1 adrenergic and histamine H1 receptors. Aripiprazole also exhibited moderate binding affinity for the serotonin reuptake site and no appreciable affinity for muscarinic receptors. Interaction with receptors other than dopamine and serotonin subtypes may explain some of the other clinical effects of aripiprazole. Aripiprazole doses ranging from 0.5 to 30 mg administered once a day to healthy subjects for 2 weeks produced a dose-dependent reduction in the binding of 11C-raclopride, a D2/D3 receptor ligand, to the caudate and putamen detected by positron emission tomography. Clinical efficacy and safety Schizophrenia In three short-term (4 to 6 weeks) placebo-controlled trials involving 1,228 schizophrenic adult patients, presenting with positive or negative symptoms, aripiprazole was associated with statistically significantly greater improvements in psychotic symptoms compared to placebo. ABILIFY is effective in maintaining the clinical improvement during continuation therapy in adult patients who have shown an initial treatment response. In a haloperidol-controlled trial, the proportion of responder patients maintaining response to medicinal product at 52-weeks was similar in both groups (aripiprazole 77 % and haloperidol 73 %). The overall completion rate was significantly higher for patients on aripiprazole (43 %) than for haloperidol (30 %). Actual scores in rating scales used as secondary endpoints, including PANSS and the Montgomery-Asberg Depression Rating Scale showed a significant improvement over haloperidol. In a 26-week, placebo-controlled trial in adult stabilised patients with chronic schizophrenia, aripiprazole had significantly greater reduction in relapse rate, 34 % in aripiprazole group and 57 % in placebo. Weight gain: in clinical trials aripiprazole has not been shown to induce clinically relevant weight gain. In a 26-week, olanzapine-controlled, double-blind, multi-national study of schizophrenia which included 314 adult patients and where the primary end-point was weight gain, significantly less patients had at least 7 % weight gain over baseline (i.e. a gain of at least 5.6 kg for a mean baseline weight of ~80.5 kg) on aripiprazole (n = 18, or 13 % of evaluable patients), compared to olanzapine (n = 45, or 33 % of evaluable patients). Lipid parameters: in a pooled analysis on lipid parameters from placebo controlled clinical trials in adults, aripiprazole has not been shown to induce clinically relevant alterations in levels of total cholesterol, triglycerides, HDL and LDL. -Total cholesterol: incidence of changes in levels from normal (<5.18 mmol/l) to high (≥ 6.22 mmol/l) was 2.5 % for aripiprazole and 2.8 % for placebo and mean change from baseline was -0.15 mmol/l (95 % CI: -0.182, -0.115) for aripiprazole and -0.11 mmol/l (95 % CI: -0.148, -0.066) for placebo. -Fasting triglycerides: incidence of changes in levels from normal (<1.69 mmol/l) to high (≥ 2.26 mmol/l) was 7.4 % for aripiprazole and 7.0 % for placebo and mean change from baseline was -0.11 mmol/l (95 % CI: -0.182, -0.046) for aripiprazole and -0.07 mmol/l (95 % CI: -0.148, 0.007) for placebo. -HDL: incidence of changes in levels from normal (≥ 1.04 mmol/l) to low (<1.04 mmol/l) was 11.4 % for aripiprazole and 12.5 % for placebo and mean change from baseline was -0.03 mmol/l (95 % CI: -0.046, -0.017) for aripiprazole and -0.04 mmol/l (95 % CI: -0.056, -0.022) for placebo. -Fasting LDL: incidence of changes in levels from normal (<2.59 mmol/l) to high (≥ 4.14 mmol/l) was 0.6 % for aripiprazole and 0.7 % for placebo and mean change from baseline was -0.09 mmol/l (95 % CI: -0.139, -0.047) for aripiprazole and -0.06 mmol/l (95 % CI: -0.116, -0.012) for placebo. Manic episodes in Bipolar I Disorder In two 3-week, flexible-dose, placebo-controlled monotherapy trials involving patients with a manic or mixed episode of Bipolar I Disorder, aripiprazole demonstrated superior efficacy to placebo in reduction of manic symptoms over 3 weeks. These trials included patients with or without psychotic features and with or without a rapid-cycling course. In one 3-week, fixed-dose, placebo-controlled monotherapy trial involving patients with a manic or mixed episode of Bipolar I Disorder, aripiprazole failed to demonstrate superior efficacy to placebo. In two 12-week, placebo- and active-controlled monotherapy trials in patients with a manic or mixed episode of Bipolar I Disorder, with or without psychotic features, aripiprazole demonstrated superior efficacy to placebo at week 3 and a maintenance of effect comparable to lithium or haloperidol at week 12. Aripiprazole also demonstrated a comparable proportion of patients in symptomatic remission from mania as lithium or haloperidol at week 12. In a 6-week, placebo-controlled trial involving patients with a manic or mixed episode of Bipolar I Disorder, with or without psychotic features, who were partially non-responsive to lithium or valproate monotherapy for 2 weeks at therapeutic serum levels, the addition of aripiprazole as adjunctive therapy resulted in superior efficacy in reduction of manic symptoms than lithium or valproate monotherapy. In a 26-week, placebo-controlled trial, followed by a 74-week extension, in manic patients who achieved remission on aripiprazole during a stabilization phase prior to randomization, aripiprazole demonstrated superiority over placebo in preventing bipolar recurrence, primarily in preventing recurrence into mania but failed to demonstrate superiority over placebo in preventing recurrence into depression. In a 52-week, placebo-controlled trial, in patients with a current manic or mixed episode of Bipolar I Disorder who achieved sustained remission (Y-MRS and MADRS total scores ≤ 12) on aripiprazole (10 mg/day to 30 mg/day) adjunctive to lithium or valproate for 12 consecutive weeks, adjunctive aripiprazole demonstrated superiority over placebo with a 46 % decreased risk (hazard ratio of 0.54) in preventing bipolar recurrence and a 65 % decreased risk (hazard ratio of 0.35) in preventing recurrence into mania over adjunctive placebo but failed to demonstrate superiority over placebo in preventing recurrence into depression. Adjunctive aripiprazole demonstrated superiority over placebo on the secondary outcome measure, CGI-BP Severity of Illness score (mania). In this trial, patients were assigned by investigators with either open-label lithium or valproate monotherapy to determine partial non-response. Patients were stabilised for at least 12 consecutive weeks with the combination of aripiprazole and the same mood stabilizer. Stabilized patients were then randomised to continue the same mood stabilizer with double-blind aripiprazole or placebo. Four mood stabilizer subgroups were assessed in the randomised phase: aripiprazole + lithium; aripiprazole + valproate; placebo + lithium; placebo + valproate. The Kaplan-Meier rates for recurrence to any mood episode for the adjunctive treatment arm were 16 % in aripiprazole + lithium and 18 % in aripiprazole + valproate compared to 45 % in placebo + lithium and 19 % in placebo + valproate. Paediatric population Schizophrenia in adolescents In a 6-week placebo-controlled trial involving 302 schizophrenic adolescent patients (13-17 years), presenting with positive or negative symptoms, aripiprazole was associated with statistically significantly greater improvements in psychotic symptoms compared to placebo. In a sub-analysis of the adolescent patients between the ages of 15 to 17 years, representing 74 % of the total enrolled population, maintenance of effect was observed over the 26-week open-label extension trial. Manic episodes in Bipolar I Disorder in children and adolescents Aripiprazole was studied in a 30-week placebo-controlled trial involving 296 children and adolescents (10-17 years), who met DSM-IV criteria for Bipolar I Disorder with manic or mixed episodes with or without psychotic features and had a Y-MRS score ≥ 20 at baseline. Among the patients included in the primary efficacy analysis, 139 patients had a current co-morbid diagnosis of ADHD. Aripiprazole was superior to placebo in change from baseline at week 4 and at week 12 on the Y-MRS total score. In a post-hoc analysis, the improvement over placebo was more pronounced in the patients with associated co-morbidity of ADHD compared to the group without ADHD, where there was no difference from placebo. Recurrence prevention was not established. Table 1: Mean improvement from baseline YMRS score by psychiatric comorbidity
b n = 46 at Week 4 The most common treatment-emergent adverse events among patients receiving 30 mg were extrapyramidal disorder (28.3 %), somnolence (27.3 %), headache (23.2 %), and nausea (14.1 %). Mean weight gain in the 30 weeks treatment-interval was 2.9 kg as compared to 0.98 kg in patients treated with placebo. Irritability associated with autistic disorder in paediatric patients (see section 4.2) Aripiprazole was studied in patients aged 6 to 17 years in two 8-week, placebo-controlled trials [one flexible-dose (2-15 mg/day) and one fixed-dose (5, 10, or 15 mg/day)] and in one 52-week open-label trial. Dosing in these trials was initiated at 2 mg/day, increased to 5 mg/day after one week, and increased by 5 mg/day in weekly increments to the target dose. Over 75 % of patients were less than 13 years of age. Aripiprazole demonstrated statistically superior efficacy compared to placebo on the Aberrant Behaviour Checklist Irritability subscale. However, the clinical relevance of this finding has not been established. The safety profile included weight gain and changes in prolactin levels. The duration of the long-term safety study was limited to 52 weeks. In the pooled trials, the incidence of low serum prolactin levels in females (<3 ng/ml) and males (<2 ng/ml) in aripiprazole-treated patients was 27/46 (58.7 %) and 258/298 (86.6 %), respectively. In the placebo-controlled trials, the mean weight gain was 0.4 kg for placebo and 1.6 kg for aripiprazole. Aripiprazole was also studied in a placebo-controlled, long-term maintenance trial. After a 13-26 week stabilisation on aripiprazole (2-15 mg/day) patients with a stable response were either maintained on aripiprazole or substituted to placebo for further 16 weeks. Kaplan-Meier relapse rates at week 16 were 35 % for aripiprazole and 52 % for placebo; the hazard ratio for relapse within 16 weeks (aripiprazole/placebo) was 0.57 (non-statistically significant difference). The mean weight gain over the stabilisation phase (up to 26 weeks) on aripiprazole was 3.2 kg, and a further mean increase of 2.2 kg for aripiprazole as compared to 0.6 kg for placebo was observed in the second phase (16 weeks) of the trial. Extrapyramidal symptoms were mainly reported during the stabilisation phase in 17 % of patients, with tremor accounting for 6.5%. Tics associated with Tourette's disorder in paediatric patients (see section 4.2) The efficacy of aripiprazole was studied in paediatric subjects with Tourette's disorder (aripiprazole: n = 99, placebo: n = 44) in a randomised, double-blind, placebo controlled, 8 week study using a fixed dose weight-based treatment group design over the dose range of 5 mg/day to 20 mg/day and a starting dose of 2 mg. Patients were 7 - 17 years of age and presented an average score of 30 on Total Tic Score on the Yale Global Tic Severity Scale (TTS-YGTSS) at baseline. Aripiprazole showed an improvement on TTS-YGTSS change from baseline to Week 8 of 13.35,for the low dose group (5 mg or 10 mg) and 16.94 for the high dose group (10 mg or 20 mg) as compared with an improvement of 7.09 in the placebo group. The efficacy of aripiprazole in paediatric subjects with Tourette's syndrome (aripiprazole: n = 32, placebo: n = 29) was also evaluated over a flexible dose range of 2 mg/day to 20 mg/day and a starting dose of 2 mg, in a 10 week, randomised, double blind, placebo-controlled study conducted in South-Korea. Patients were 6 - 18 years and presented an average score of 29 on TTS-YGTSS at baseline. Aripiprazole group showed an improvement of 14.97 on TTS-YGTSS change from baseline to Week 10 as compared with an improvement of 9.62 in the placebo group. In both of these short term trials, the clinical relevance of the efficacy findings has not been established, considering the magnitude of treatment effect compared to the large placebo effect and the unclear effects regarding psycho-social functioning. No long term data are available with regard to the efficacy and the safety of aripiprazole in this fluctuating disorder. The European Medicines Agency has deferred the obligation to submit the results of studies with ABILIFY in one or more subsets of the paediatric population in the treatment of schizophrenia and in the treatment of bipolar affective disorder (see section 4.2 for information on paediatric use). 5.2 Pharmacokinetic properties Absorption Aripiprazole is well absorbed, with peak plasma concentrations occurring within 3-5 hours after dosing. Aripiprazole undergoes minimal pre-systemic metabolism. The absolute oral bioavailability of the tablet formulation is 87 %. There is no effect of a high fat meal on the pharmacokinetics of aripiprazole. Distribution Aripiprazole is widely distributed throughout the body with an apparent volume of distribution of 4.9 l/kg, indicating extensive extravascular distribution. At therapeutic concentrations, aripiprazole and dehydro-aripiprazole are greater than 99 % bound to serum proteins, binding primarily to albumin. Biotransformation Aripiprazole is extensively metabolised by the liver primarily by three biotransformation pathways: dehydrogenation, hydroxylation, and N-dealkylation. Based on in vitro studies, CYP3A4 and CYP2D6 enzymes are responsible for dehydrogenation and hydroxylation of aripiprazole, and N-dealkylation is catalysed by CYP3A4. Aripiprazole is the predominant medicinal product moiety in systemic circulation. At steady state, dehydro-aripiprazole, the active metabolite, represents about 40 % of aripiprazole AUC in plasma. Elimination The mean elimination half-lives for aripiprazole are approximately 75 hours in extensive metabolisers of CYP2D6 and approximately 146 hours in poor metabolisers of CYP2D6. The total body clearance of aripiprazole is 0.7 ml/min/kg, which is primarily hepatic. Following a single oral dose of [14C]-labelled aripiprazole, approximately 27 % of the administered radioactivity was recovered in the urine and approximately 60 % in the faeces. Less than 1 % of unchanged aripiprazole was excreted in the urine and approximately 18 % was recovered unchanged in the faeces. Pharmacokinetics in special patient groups Paediatric population The pharmacokinetics of aripiprazole and dehydro-aripiprazole in paediatric patients 10 to 17 years of age were similar to those in adults after correcting for the differences in body weights. Older people There are no differences in the pharmacokinetics of aripiprazole between healthy elderly and younger adult subjects, nor is there any detectable effect of age in a population pharmacokinetic analysis in schizophrenic patients. Gender There are no differences in the pharmacokinetics of aripiprazole between healthy male and female subjects nor is there any detectable effect of gender in a population pharmacokinetic analysis in schizophrenic patients. Smoking and Race Population pharmacokinetic evaluation has revealed no evidence of clinically significant race-related differences or effects from smoking upon the pharmacokinetics of aripiprazole. Renal impairment The pharmacokinetic characteristics of aripiprazole and dehydro-aripiprazole were found to be similar in patients with severe renal disease compared to young healthy subjects. Hepatic impairment A single-dose study in subjects with varying degrees of liver cirrhosis (Child-Pugh Classes A, B, and C) did not reveal a significant effect of hepatic impairment on the pharmacokinetics of aripiprazole and dehydro-aripiprazole, but the study included only 3 patients with Class C liver cirrhosis, which is insufficient to draw conclusions on their metabolic capacity. 5.3 Preclinical safety data Non-clinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity, carcinogenic potential, toxicity to reproduction and development. Toxicologically significant effects were observed only at doses or exposures that were sufficiently in excess of the maximum human dose or exposure, indicating that these effects were limited or of no relevance to clinical use. These included: dose-dependent adrenocortical toxicity (lipofuscin pigment accumulation and/or parenchymal cell loss) in rats after 104 weeks at 20 to 60 mg/kg/day (3 to 10 times the mean steady-state AUC at the maximum recommended human dose) and increased adrenocortical carcinomas and combined adrenocortical adenomas/carcinomas in female rats at 60 mg/kg/day (10 times the mean steady-state AUC at the maximum recommended human dose). The highest nontumorigenic exposure in female rats was 7 times the human exposure at the recommended dose. An additional finding was cholelithiasis as a consequence of precipitation of sulphate conjugates of hydroxy metabolites of aripiprazole in the bile of monkeys after repeated oral dosing at 25 to 125 mg/kg/day (1 to 3 times the mean steady-state AUC at the maximum recommended clinical dose or 16 to 81 times the maximum recommended human dose based on mg/m2). However, the concentrations of the sulphate conjugates of hydroxy aripiprazole in human bile at the highest dose proposed, 30 mg per day, were no more than 6 % of the bile concentrations found in the monkeys in the 39-week study and are well below (6 %) their limits of in vitro solubility. In repeat-dose studies in juvenile rats and dogs, the toxicity profile of aripiprazole was comparable to that observed in adult animals, and there was no evidence of neurotoxicity or adverse effects on development. Based on results of a full range of standard genotoxicity tests, aripiprazole was considered non-genotoxic. Aripiprazole did not impair fertility in reproductive toxicity studies. Developmental toxicity, including dose-dependent delayed foetal ossification and possible teratogenic effects, were observed in rats at doses resulting in subtherapeutic exposures (based on AUC) and in rabbits at doses resulting in exposures 3 and 11 times the mean steady-state AUC at the maximum recommended clinical dose. Maternal toxicity occurred at doses similar to those eliciting developmental toxicity. 6. Pharmaceutical particulars 6.1 List of excipients Lactose monohydrate Maize starch Microcrystalline cellulose Hydroxypropyl cellulose Magnesium stearate Indigo carmine aluminium lake (E132) 6.2 Incompatibilities Not applicable. 6.3 Shelf life 3 years 6.4 Special precautions for storage Store in the original package in order to protect from moisture. 6.5 Nature and contents of container Aluminium perforated unit dose blisters in cartons of 14 x 1, 28 x 1, 49 x 1, 56 x 1, 98 x 1 tablets. Not all pack sizes may be marketed. 6.6 Special precautions for disposal and other handling Any unused medicinal product or waste material should be disposed of in accordance with local requirements. 7. Marketing authorisation holder Otsuka Pharmaceutical Europe Ltd. Gallions, Wexham Springs, Framewood Road, Wexham, SL3 6PJ - United Kingdom 8. Marketing authorisation number(s) EU/1/04/276/001-005 9. Date of first authorisation/renewal of the authorisation Date of first authorisation: 04 June 2004 Date of latest renewal: 04 June 2009 10. Date of revision of the text 04/2015 Detailed information on this medicinal product is available on the website of the European Medicines Agency http://www.ema.europa.eu. 附: Abilify 10mg orodispersible tablets(http://www.medicines.org.uk/emc/medicine/30374) Abilify 10mg tablets(http://www.medicines.org.uk/emc/medicine/30369) Abilify 15mg orodispersible tablets(http://www.medicines.org.uk/emc/medicine/30381) Abilify 15mg tablets(http://www.medicines.org.uk/emc/medicine/30378) Abilify 30mg tablets(http://www.medicines.org.uk/emc/medicine/30375) Abilify 7.5 mg/ml solution for injection (intramuscular)(http://www.medicines.org.uk/emc/medicine/20802) Abilify Maintena 400 mg powder and solvent for prolonged-release suspension for injection(http://www.medicines.org.uk/emc/medicine/28494) Abilify oral solution(http://www.medicines.org.uk/emc/medicine/30380) |
阿立哌唑片|Abilify(Aripiprazole Tablets)简介:
英文药名: Abilify(Aripiprazole Tablets)
中文药名: 阿立哌唑片
生产厂家: 大冢制药/百时美施贵宝药品介绍中文药名: 阿立哌唑英文药名: Abilify (Aripiprazole Tablets) 生产厂家Otsuka America Pha ... 责任编辑:admin |
最新文章更多推荐文章更多热点文章更多
|